北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (5): 870-874. doi: 10.19723/j.issn.1671-167X.2020.05.012
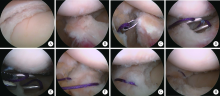
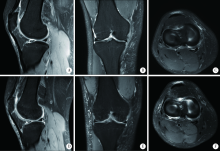
关节镜下改良outside-in穿刺缝合技术修复半月板撕裂的中期临床随访
- 北京大学人民医院创伤救治中心,北京大学人民医院创伤骨科,北京 100044
A mid-term clinical follow-up study on repair of the meniscus tears by a modified arthroscopic outside-in puncture suture technique
Zhong-di LIU,Ting-min XU,Yu DANG( ),Dian-ying ZHANG,Zhong-guo FU
),Dian-ying ZHANG,Zhong-guo FU
- Trauma Medicine Center, Department of Trauma and Orthopaedics, Peking University People’s Hospital, Beijing 100044, China
摘要:
目的:探讨关节镜下利用腰椎穿刺针结合outside-in缝合技术治疗膝关节半月板撕裂的临床疗效。方法:选择2015年1月至2017年10月因半月板撕裂采用关节镜下利用腰椎穿刺针结合outside-in缝合技术治疗的患者的病例资料进行回顾性分析。共纳入病例95例,男36例,女59例;年龄16~77岁,平均(46.79±18.07)岁;左侧53例,右侧42例,致伤原因包括运动、扭伤等。根据Barrett标准判断半月板临床愈合情况,采用Lysholm评分、膝关节活动度、视觉模拟评分(visual analogue scale, VAS)、膝关节磁共振对患者术后膝关节功能及康复情况进行评估。结果:95例患者随访时间22~36 个月,平均(28.32±3.98)个月。根据Barrett标准,90例(94.7%)患者获得半月板临床愈合。对比术前与术后患者膝关节Lysholm评分、关节活动度和VAS评分,差异均有统计学意义(P<0.01)。随访过程中未发现手术部位感染、关节周围血管神经损伤、线结反应等并发症。结论:采用关节镜下腰椎穿刺针结合outside-in缝合技术治疗半月板前角及体部撕裂具有操作简单、创伤小、恢复快的特点,临床效果满意,可能是治疗半月板前角及体部撕裂的有效办法。
中图分类号:
- R684
| [1] |
Kurzweil PR, Cannon WD, DeHaven KE. Meniscus repair and replacement[J]. Sports Med Arthrosc Rev, 2018,26(4):160-164.
doi: 10.1097/JSA.0000000000000224 pmid: 30395058 |
| [2] |
Vaquero-Picado A, Rodríguez-Merchín EC. Arthroscopic repair of the meniscus: surgical management and clinical outcomes[J]. EFORT Open Rev, 2018,3(11):584-594.
doi: 10.1302/2058-5241.3.170059 pmid: 30595844 |
| [3] |
Karia M, Ghaly Y, Al-Hadithy N, et al. Current concepts in the techniques, indications and outcomes of meniscal repairs[J]. Eur J Orthop Surg Traumatol, 2019,29(3):509-520.
doi: 10.1007/s00590-018-2317-5 pmid: 30374643 |
| [4] |
Steiner S, Feeley SM, Ruland JR, et al. Outside-in repair technique for a complete radial tear of the lateral meniscus[J]. Arthrosc Tech, 2018,7(3):e285-e288.
doi: 10.1016/j.eats.2017.09.006 pmid: 29881702 |
| [5] |
Barrett GR, Treacy SH, Ruff CG. Preliminary results of the T-fix endoscopic meniscus repair technique in an anterior cruciate ligament reconstruction population[J]. Arthroscopy, 1997,13(2):218-223.
doi: 10.1016/s0749-8063(97)90157-2 pmid: 9127080 |
| [6] |
Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale[J]. Am J Sports Med, 1982,10(3):150-154.
doi: 10.1177/036354658201000306 pmid: 6896798 |
| [7] |
Fox AJ, Wanivenhaus F, Burge AJ, et al. The human meniscus: a review of anatomy, function, injury, and advances in treatment[J]. Clin Anat, 2015,28(2):269-287.
doi: 10.1002/ca.22456 pmid: 25125315 |
| [8] |
Ouyang X, Wei B, Hong SD, et al. Arthroscopic characteristics of normal and discoid meniscus injury, and efficiency of recovery in each type of meniscus injury[J]. Cell Biochem Biophys, 2015,72(2):433-437.
doi: 10.1007/s12013-014-0483-6 pmid: 25572056 |
| [9] |
Badlani JT, Borrero C, Golla S, et al. The effects of meniscus injury on the development of knee osteoarthritis: data from the osteoarthritis initiative[J]. Am J Sports Med, 2013,41(6):1238-1244.
pmid: 23733830 |
| [10] |
Rai MF, Brophy RH, Sandell LJ. Osteoarthritis following meniscus and ligament injury: insights from translational studies and animal models[J]. Curr Opin Rheumatol, 2019,31(1):70-79.
doi: 10.1097/BOR.0000000000000566 pmid: 30394938 |
| [11] |
Rai MF, McNulty AL. Meniscus beyond mechanics: Using biology to advance our understanding of meniscus injury and treatment[J]. Connect Tissue Res, 2017,58(3/4):221-224.
doi: 10.1080/03008207.2017.1312921 |
| [12] |
Twomey-Kozak J, Jayasuriya CT. Meniscus repair and regeneration: a systematic review from a basic and translational science perspective[J]. Clin Sports Med, 2020,39(1):125-163.
doi: 10.1016/j.csm.2019.08.003 pmid: 31767102 |
| [13] | Muniandy M, Rajagopal S, Tahir SH. Arthroscopic all-inside repair of tear of the anterior horn of discoid lateral meniscus[J]. Surg J (NY), 2019,5(1):e35-e37. |
| [14] |
Muckenhirn KJ, Kruckeberg BM, Cinque ME, et al. Arthroscopic inside-out repair of a meniscus bucket-handle tear augmented with bone marrow aspirate concentrate[J]. Arthrosc Tech, 2017,6(4):e1221-e1227.
doi: 10.1016/j.eats.2017.04.014 pmid: 29354421 |
| [15] |
Marinescu R, Laptoiu D, Negrusoiu M. Outside-in meniscus suture technique: 5 years' follow-up[J]. Knee Surg Sports Traumatol Arthrosc, 2003,11(3):167-172.
doi: 10.1007/s00167-003-0347-x pmid: 12774154 |
| [1] | 王江静,魏顺依,敖英芳,杨渝平. 前交叉韧带重建术后三种不同药物镇痛早期疗效的对比[J]. 北京大学学报(医学版), 2024, 56(2): 293-298. |
| [2] | 安思兰,郑群怡,王锴,高姗. 全膝关节置换术后患者早期疼痛的特点及其影响因素[J]. 北京大学学报(医学版), 2024, 56(1): 167-173. |
| [3] | 董寒梅,吴睿麒,高冠英,刘镕阁,徐雁. 关节镜下盂唇重建治疗髋关节撞击综合征12例[J]. 北京大学学报(医学版), 2021, 53(5): 1007-1011. |
| [4] | 苗欣,黄红拾,胡晓青,时会娟,任爽,敖英芳. 膝关节前交叉韧带断裂后单腿位置觉测试时脑电功率谱的变化特征[J]. 北京大学学报(医学版), 2021, 53(5): 871-876. |
| [5] | 吴浩,潘利平,刘恒,塔拉提百克·买买提居马,王洪彬,宁太国,曹永平. 胫骨假体的不同后倾角度对内侧间室单髁置换术后膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 877-882. |
| [6] | 印钰,梅宇,王泽刚,宋首一,刘鹏飞,何鹏峰,武文杰,谢兴. 固定袢和可调节袢在粗骨道中的长度对股骨骨道增宽及膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 883-890. |
| [7] | 郑佳鹏,肖棋,邓辉云,吴清泉,翟文亮,林达生. 外侧半月板腘肌腱区损伤的关节镜下分型和处理[J]. 北京大学学报(医学版), 2021, 53(5): 891-895. |
| [8] | 邵振兴,宋庆法,赵宇晴,崔国庆. 一种结合线袢固定的关节镜下“嵌入式”喙突移位术:手术技术及术后影像学分析[J]. 北京大学学报(医学版), 2021, 53(5): 896-901. |
| [9] | 王鑫光,耿霄,李杨,吴天晨,李子剑,田华. 便携式导航与计算机导航辅助在全膝关节置换力线对准和手术时间的比较[J]. 北京大学学报(医学版), 2021, 53(4): 728-733. |
| [10] | 江东,胡跃林,焦晨,郭秦炜,谢兴,陈临新,赵峰,皮彦斌. 慢性踝关节不稳合并后踝撞击同期手术中长期疗效及影响因素分析[J]. 北京大学学报(医学版), 2019, 51(3): 505-509. |
| [11] | 张翠平,刘佩佩,傅强,高冠英,崔立刚,徐雁,王健全. 超声引导下髋关节药物注射在关节镜盂唇修复术后康复中的应用[J]. 北京大学学报(医学版), 2019, 51(2): 265-267. |
| [12] | 刘晓东,崔立刚,徐雁,孙洋,郝云霞,宋琳. 超声在髋关节前上盂唇撕裂中的应用[J]. 北京大学学报(医学版), 2017, 49(6): 1014-1018. |
| [13] | 王军锋, 李沼, 张克石, 袁峰, 李儒军, 钟群杰, 关振鹏. 双膝关节置换术中髌骨置换与否的左右侧随机对照研究[J]. 北京大学学报(医学版), 2017, 49(5): 861-866. |
| [14] | 李杨,李子剑,张克,田华,刘延青,蔡宏,李锋,赵旻暐. 膝髋关节置换术非计划性暂停手术的原因分析[J]. 北京大学学报(医学版), 2017, 49(2): 231-235. |
| [15] | 赵旻暐, 王宁, 曾琳, 李民, 赵中凯, 张菡, 田华. 膝关节置换术后连续收肌管阻滞与股神经阻滞的疗效比较[J]. 北京大学学报(医学版), 2017, 49(1): 142-147. |
|
||