北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (1): 120-125. doi: 10.19723/j.issn.1671-167X.2021.01.018
玻璃体和通用型复合树脂耐磨性的临床对照研究
- 1.北京大学口腔医学院·口腔医院,牙体牙髓科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
2.北京大学口腔医学院·口腔医院第一门诊部综合科,北京 100034
Evaluation of wear property of Giomer and universal composite in vivo
MU Hai-li1,2,TIAN Fu-cong3,WANG Xiao-yan1,Δ( ),GAO Xue-jun1
),GAO Xue-jun1
- 1. Department of Cariology and Endodontology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. First Clinical Division, Peking University School and Hospital of Stomatology, Beijing 100034, China
摘要:
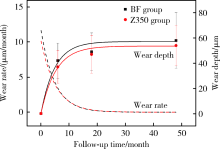
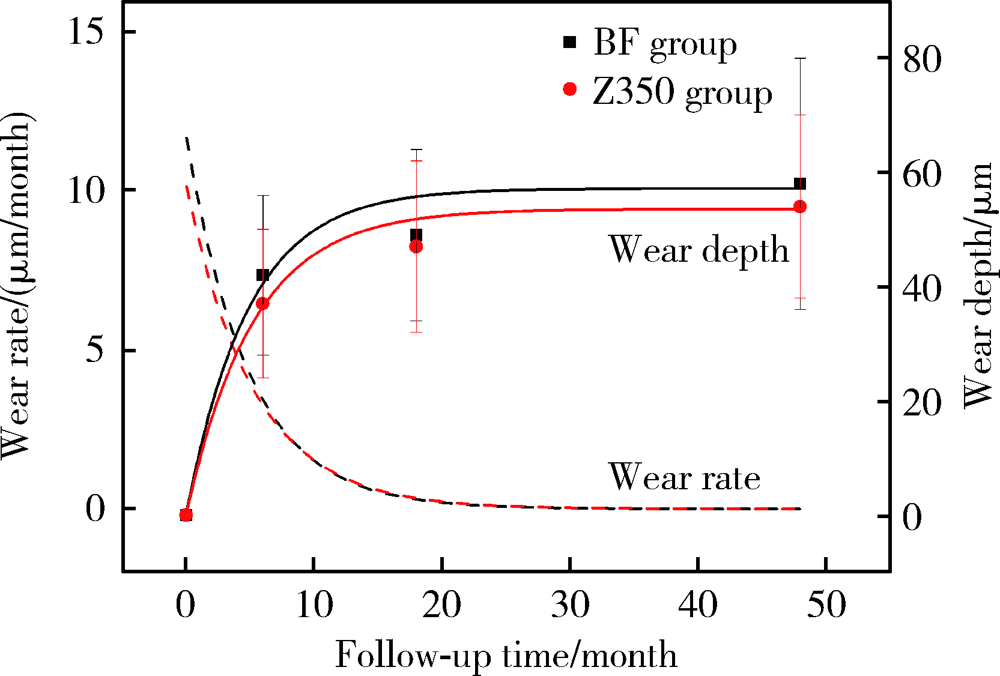
目的: 采用激光三维扫描技术评估玻璃体和通用型复合树脂用于后牙充填的耐磨性。方法: 根据纳入标准选取48名患者共108颗患牙(每组各54颗),随机分配用玻璃体(Beautifil Ⅱ,简称BF)或通用型复合树脂(Filtek Z350,简称Z350)进行充填。分别于术后1周、6个月、18个月和4年,采用改良美国公共卫生署(United States Public Health Service,USPHS)标准对充填体进行临床评价并拍照和制取模型。使用激光三维扫描仪扫描模型后,对图像进行配准和计算磨耗深度,使用SPSS 20.0进行统计分析。结果: 术后4年回访43名患者,回访率为89.6%。BF组和Z350组各有4例和3例出现脱落、继发龋、充填体折断和牙髓坏死。两组充填体的4年存留率均为95.8%,符合美国牙医协会(American Dental Association,ADA)标准(3年存留率>90%)。0~6个月两组充填体的磨耗速率最快,随后磨耗速率的下降趋于平缓,BF组4年总磨耗深度为(58±22) μm,Z350组为(54±16) μm(P>0.05), 耐磨性均符合ADA标准(3年磨耗深度<100 μm)。两组充填体均表现为围绕咬合接触区形成凹坑状磨耗(Ⅰ型)和充填体发生均匀磨耗(Ⅱ型)。术后4年,Ⅰ型磨耗充填体中,BF组的磨耗深度大于Z350组(P<0.05),Ⅱ型磨耗充填体中,两组间差异无统计学意义(P>0.05)。结论: 玻璃体的4年存留率和耐磨性均符合ADA标准,用于后牙牙合面重咬合接触区时,玻璃体的耐磨性略逊于复合树脂,用于非重咬合接触区时,二者间无明显差异。
中图分类号:
- R783.1
| [1] | Gordan VV, Blaser PK, Watson RE, et al. A clinical evaluation of a giomer restorative system containing surface prereacted glass ionomer filler: results from a 13-year recall examination[J]. J Am Dent Assoc, 2014,145(10):1036-1043. |
| [2] |
Manhart J, Chen HY, Hickel R. Clinical evaluation of the poste-rior composite Quixfil in class Ⅰ and Ⅱ cavities: 4-year follow-up of a randomized controlled trial[J]. J Adhes Dent, 2010,12(3):237-243.
doi: 10.3290/j.jad.a17551 pmid: 20157663 |
| [3] |
Oz FD, Ergin E, Canatan S. Twenty-four-month clinical perfor-mance of different universal adhesives in etch-and-rinse, selective etching and self-etch application modes in NCCL: a randomized controlled clinical trial[J]. J Appl Oral Sci, 2019,27:e20180358.
doi: 10.1590/1678-7757-2018-0358 pmid: 30994773 |
| [4] |
Koc Vural U, Meral E, Ergin E, et al. Twenty-four-month clinical performance of a glass hybrid restorative in non-carious cervical lesions of patients with bruxism: a split-mouth, randomized clinical trial[J]. Clin Oral Investig, 2020,24(3):1229-1238.
doi: 10.1007/s00784-019-02986-x pmid: 31297658 |
| [5] |
Hayashi M, Wilson NH. Failure risk of posterior composites with post-operative sensitivity[J]. Oper Dent, 2003,28(6):681-688.
pmid: 14653280 |
| [6] |
Heintze SD. Clinical relevance of tests on bond strength, microleakage and marginal adaptation[J]. Dent Mater, 2013,29(1):59-84.
doi: 10.1016/j.dental.2012.07.158 |
| [7] |
Naoum S, Ellakwa A, Martin F, et al. Fluoride release, recharge and mechanical property stability of various fluoride-containing resin composites[J]. Oper Dent, 2011,36(4):422-432.
doi: 10.2341/10-414-L pmid: 21819201 |
| [8] |
Ikemura K, Tay FR, Endo T, et al. A review of chemical-approach and ultramorphological studies on the development of fluoride-releasing dental adhesives comprising new pre-reacted glass ionomer (PRG) fillers[J]. Dent Mater J, 2008,27(3):315-339.
doi: 10.4012/dmj.27.315 pmid: 18717159 |
| [9] |
Saku S, Kotake H, Scougall-Vilchis RJ, et al. Antibacterial acti-vity of composite resin with glass-ionomer filler particles[J]. Dent Mater J, 2010,29(2):193-198.
doi: 10.4012/dmj.2009-050 pmid: 20379030 |
| [10] |
Kitagawa H, Miki-Oka S, Mayanagi G, et al. Inhibitory effect of resin composite containing S-PRG filler on Streptococcus mutans glucose metabolism[J]. J Dent, 2018,70:92-96.
doi: 10.1016/j.jdent.2017.12.017 pmid: 29294301 |
| [11] |
Kakuta K, Wonglamsam A, Goto S, et al. Surface textures of composite resins after combined wear test simulating both occlusal wear and brushing wear[J]. Dent Mater J, 2012,31(1):61-67.
doi: 10.4012/dmj.2010-091 |
| [12] |
Ruivo MA, Pacheco RR, Sebold M, et al. Surface roughness and filler particles characterization of resin-based composites[J]. Microsc Res Tech, 2019,82(10):1756-1767.
doi: 10.1002/jemt.23342 pmid: 31313442 |
| [13] |
Condo R, Cerroni L, Pasquantonio G, et al. A deep morphological characterization and comparison of different dental restorative materials[J]. Biomed Res Int, 2017,2017:7346317.
doi: 10.1155/2017/7346317 pmid: 28752095 |
| [14] |
Heintze SD, Faouzi M, Rousson V, et al. Correlation of wear in vivo and six laboratory wear methods[J]. Dent Mater, 2012,28(9):961-973.
doi: 10.1016/j.dental.2012.04.006 |
| [15] |
Heintze SD, Ilie N, Hickel R, et al. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials: A systematic review[J]. Dent Mater, 2017,33(3):e101-e114.
doi: 10.1016/j.dental.2016.11.013 pmid: 27993372 |
| [16] |
Hickel R, Roulet JF, Bayne S, et al. Recommendations for conducting controlled clinical studies of dental restorative materials[J]. Clin Oral Investig, 2007,11(1):5-33.
doi: 10.1007/s00784-006-0095-7 pmid: 17262225 |
| [17] |
Leinfelder KF, Taylor DF, Barkmeier WW, et al. Quantitative wear measurement of posterior composite resins[J]. Dent Mater, 1986,2(5):198-201.
doi: 10.1016/S0109-5641(86)80013-6 pmid: 3468024 |
| [18] |
Mehl A, Gloger W, Kunzelmann KH, et al. A new optical 3-D device for the detection of wear[J]. J Dent Res, 1997,76(11):1799-1807.
doi: 10.1177/00220345970760111201 pmid: 9372798 |
| [19] |
Palotie U, Eronen AK, Vehkalahti K, et al. Longevity of 2- and 3-surface restorations in posterior teeth of 25- to 30-year-old attending Public Dental Service: A 13-year observation[J]. J Dent, 2017,62:13-17.
doi: 10.1016/j.jdent.2017.05.012 pmid: 28529175 |
| [20] | The American Dental Association. ADA acceptance program guidelines: resin based composites for posterior restorations [R]. Chicago: ADA Council on Scientific Affairs, 2001. |
| [21] |
Lempel E, Toth A, Fabian T, et al. Retrospective evaluation of posterior direct composite restorations: 10-year findings[J]. Dent Mater, 2015,31(2):115-122.
doi: 10.1016/j.dental.2014.11.001 pmid: 25480695 |
| [22] |
Demarco FF, Correa MB, Cenci MS, et al. Longevity of posterior composite restorations: not only a matter of materials[J]. Dent Mater, 2012,28(1):87-101.
doi: 10.1016/j.dental.2011.09.003 |
| [23] |
Hewlett ER, Orro ME, Clark GT. Accuracy testing of three-dimensional digitizing systems[J]. Dent Mater, 1992,8(1):49-53.
doi: 10.1016/0109-5641(92)90053-f pmid: 1521684 |
| [24] |
Thongthammachat S, Moore BK, Barco MT 2nd, et al. Dimensional accuracy of dental casts: influence of tray material, impression material, and time[J]. J Prosthodont, 2002,11(2):98-108.
pmid: 12087547 |
| [25] |
Palaniappan S, Bharadwaj D, Mattar DL, et al. Three-year randomized clinical trial to evaluate the clinical performance and wear of a nanocomposite versus a hybrid composite[J]. Dent Mater, 2009,25(11):1302-1314.
doi: 10.1016/j.dental.2009.06.001 |
| [26] |
Palaniappan S, Elsen L, Lijnen I, et al. Nanohybrid and microfilled hybrid versus conventional hybrid composite restorations: 5-year clinical wear performance[J]. Clin Oral Investig, 2012,16(1):181-190.
doi: 10.1007/s00784-010-0500-0 pmid: 21221678 |
| [27] |
Goldberg AJ, Rydinge E, Santucci EA, et al. Clinical evaluation methods for posterior composite restorations[J]. J Dent Res, 1984,63(12):1387-1391.
doi: 10.1177/00220345840630120901 pmid: 6239885 |
| [28] |
da Rosa Rodolpho PA, Cenci MS, Donassollo TA, et al. A clinical evaluation of posterior composite restorations: 17-year findings[J]. J Dent, 2006,34(7):427-435.
doi: 10.1016/j.jdent.2005.09.006 pmid: 16314023 |
| [29] |
Wilson NHF, Norman RD. Five-year findings of a multiclinical trial for posterior composite[J]. J Dent, 1991,19(3):153-159.
doi: 10.1016/0300-5712(91)90005-j pmid: 1939815 |
| [30] |
Satou N, Khan AM, Satou K, et al. In-vitro and in-vivo wear profile of composite resins[J]. J Oral Rehabil, 1992,19(1):31-37.
doi: 10.1111/j.1365-2842.1992.tb01588.x pmid: 1316435 |
| [31] |
Salgado VE, Cavalcante LM, Silikas N, et al. The influence of nanoscale inorganic content over optical and surface properties of model composites[J]. J Dent, 2013,41(Suppl 5):e45-53.
doi: 10.1016/j.jdent.2013.05.011 |
| [32] |
Lim BS, Ferracane JL, Condon JR, et al. Effect of filler fraction and filler surface treatment on wear of microfilled composites[J]. Dent Mater, 2002,18(1):1-11.
doi: 10.1016/S0109-5641(00)00103-2 |
| [33] |
Garoushi S, Vallittu PK, Lassila L. Characterization of fluoride releasing restorative dental materials[J]. Dent Mater J, 2018,37(2):293-300.
doi: 10.4012/dmj.2017-161 pmid: 29279547 |
| [34] |
Gonulol N, Ozer S, Sen Tunc E. Water sorption, solubility, and color stability of giomer restoratives[J]. J Esthet Restor Dent, 2015,27(5):300-306.
doi: 10.1111/jerd.12119 pmid: 25145876 |
| [35] |
Park CA, Hyun SH, Lee JH, et al. Evaluation of polymerization in fluoride-containing composite resins[J]. J Mater Sci Mater Med, 2007,18(8):1549-1556.
doi: 10.1007/s10856-007-3023-8 pmid: 17437069 |
| [1] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [2] | 田宇轩,阮明健,刘毅,李德润,吴静云,沈棋,范宇,金杰. 双参数MRI改良PI-RADS评分4分和5分病灶的最大径对临床有意义前列腺癌的预测效果[J]. 北京大学学报(医学版), 2024, 56(4): 567-574. |
| [3] | 唐祖南,胡耒豪,陈震,于尧,章文博,彭歆. 增强现实技术在口腔颌面颈部解剖识别中的应用评价[J]. 北京大学学报(医学版), 2024, 56(3): 541-545. |
| [4] | 吕梁,张铭津,温奧楠,赵一姣,王勇,李晶,杨庚辰,柳大为. 应用三维软组织空间线角模板法评价颏部对称性[J]. 北京大学学报(医学版), 2024, 56(1): 106-110. |
| [5] | 毛渤淳,田雅婧,王雪东,李晶,周彦恒. 骨性Ⅱ类高角患者拔牙矫治前后的面部软硬组织变化[J]. 北京大学学报(医学版), 2024, 56(1): 111-119. |
| [6] | 凌晓彤,屈留洋,郑丹妮,杨静,闫雪冰,柳登高,高岩. 牙源性钙化囊肿与牙源性钙化上皮瘤的三维影像特点[J]. 北京大学学报(医学版), 2024, 56(1): 131-137. |
| [7] | 刘毅,袁昌巍,吴静云,沈棋,肖江喜,赵峥,王霄英,李学松,何志嵩,周利群. 靶向穿刺+6针系统穿刺对PI-RADS 5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2023, 55(5): 812-817. |
| [8] | 袁昌巍,李德润,李志华,刘毅,山刚志,李学松,周利群. 多参数磁共振成像中动态对比增强状态在诊断PI-RADS 4分前列腺癌中的应用[J]. 北京大学学报(医学版), 2023, 55(5): 838-842. |
| [9] | 刘颖,霍然,徐慧敏,王筝,王涛,袁慧书. 磁共振血管壁成像评估颈动脉中重度狭窄患者斑块特征与脑血流灌注的相关性[J]. 北京大学学报(医学版), 2023, 55(4): 646-651. |
| [10] | 傅强,高冠英,徐雁,林卓华,孙由静,崔立刚. 无症状髋关节前上盂唇撕裂超声与磁共振检查的对比研究[J]. 北京大学学报(医学版), 2023, 55(4): 665-669. |
| [11] | 刘想,谢辉辉,许玉峰,张晓东,陶晓峰,柳林,王霄英. 人工智能对提高放射科住院医生诊断胸部肋骨骨折一致性的价值[J]. 北京大学学报(医学版), 2023, 55(4): 670-675. |
| [12] | 黄莹,吴志远,周行红,蔡志刚,张杰. 股前外侧皮瓣修复上颌骨缺损术后面部软组织对称性感观分级[J]. 北京大学学报(医学版), 2023, 55(4): 708-715. |
| [13] | 张雯,刘筱菁,李自力,张益. 基于解剖标志的鼻翼基底缩窄缝合术对正颌患者术后鼻唇部形态的影响[J]. 北京大学学报(医学版), 2023, 55(4): 736-742. |
| [14] | 欧蒙恩,丁云,唐卫峰,周永胜. 基台边缘-牙冠的平台转移结构中粘接剂流动的三维有限元分析[J]. 北京大学学报(医学版), 2023, 55(3): 548-552. |
| [15] | 温奥楠,刘微,柳大为,朱玉佳,萧宁,王勇,赵一姣. 5种椅旁三维颜面扫描技术正确度的初步评价[J]. 北京大学学报(医学版), 2023, 55(2): 343-350. |
|
||