北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (1): 109-119. doi: 10.19723/j.issn.1671-167X.2021.01.017
不同垂直骨面型骨性Ⅱ类青少年女性颞下颌关节锥形束CT测量分析
- 北京大学口腔医学院·口腔医院,正畸科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
Cone-beam CT evaluation of temporomandibular joint in skeletal class Ⅱ female adolescents with different vertical patterns
- Department of Orthodontics, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
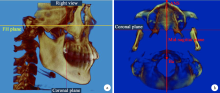
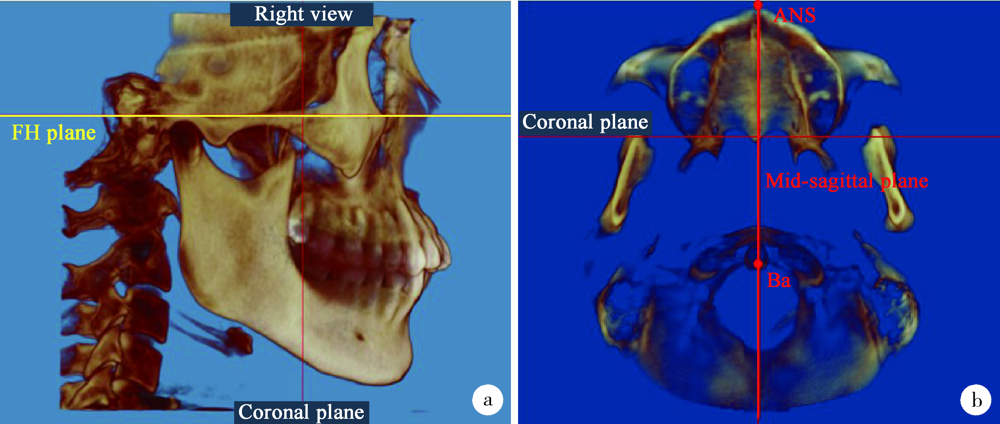
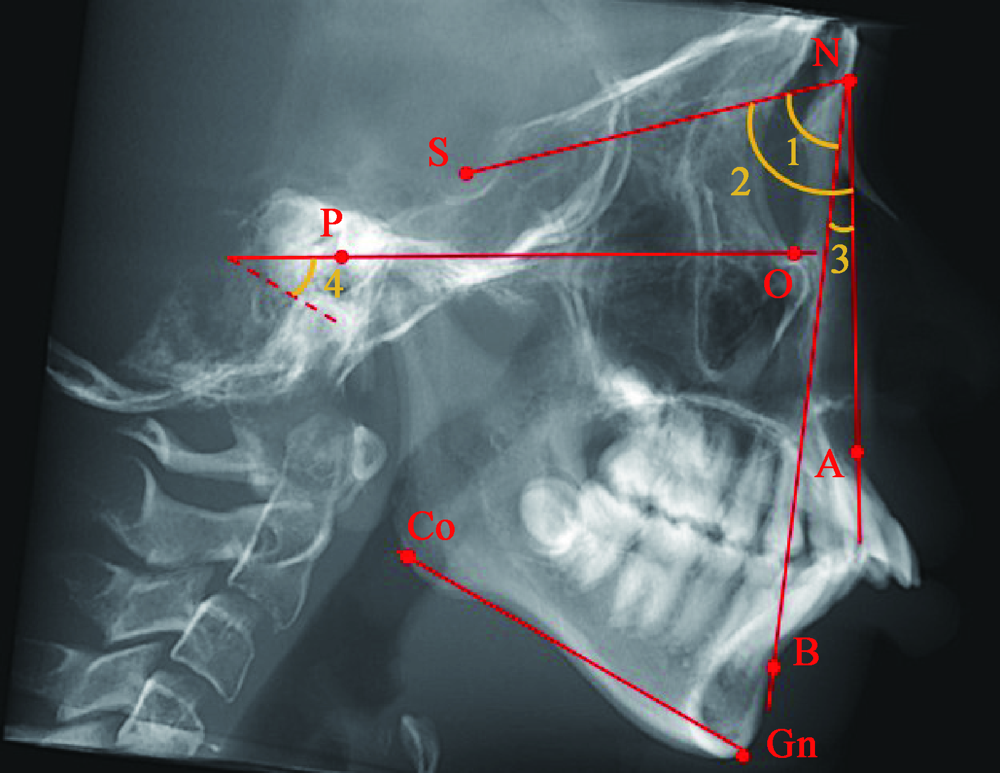
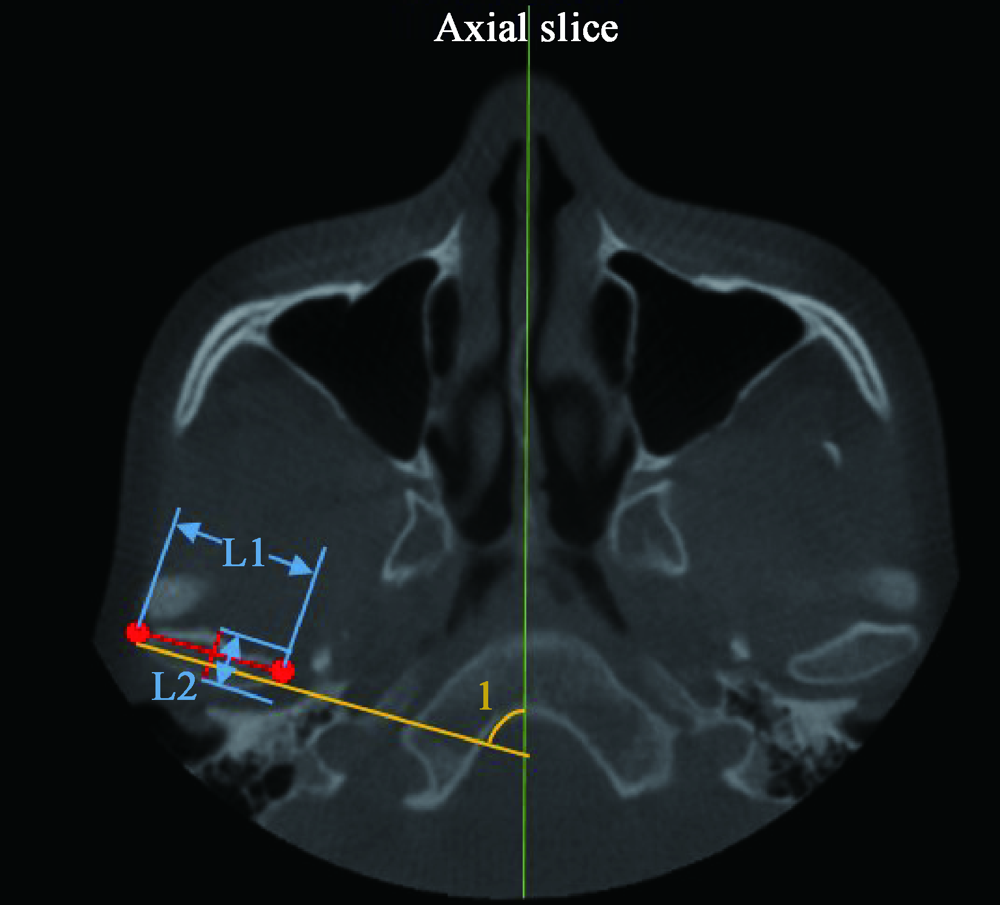
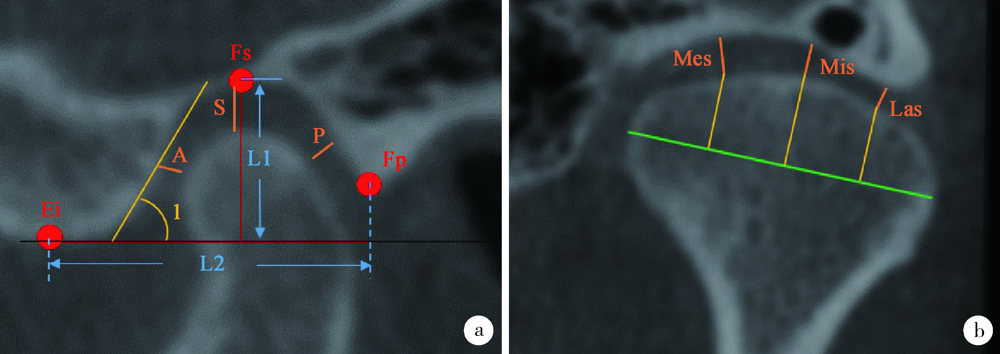
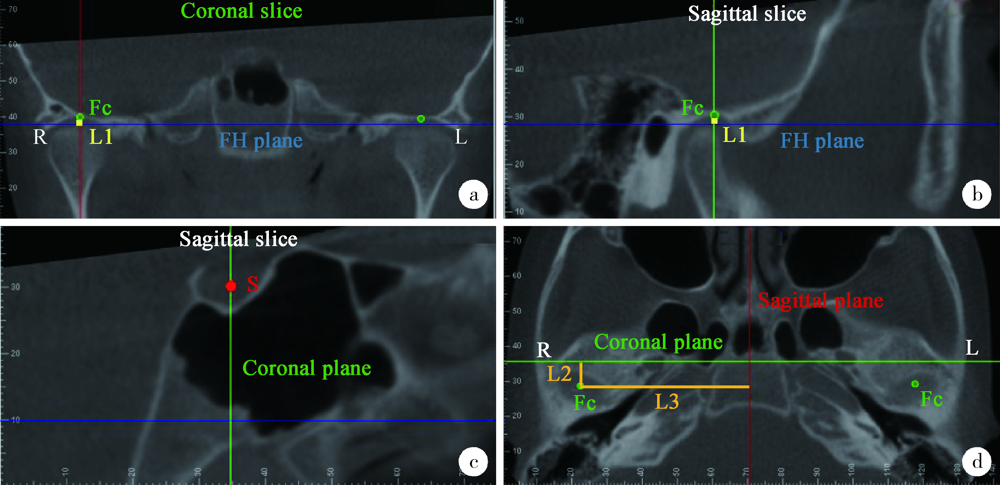
目的: 探讨不同垂直骨面型骨性Ⅱ类青少年女性颞下颌关节形态和位置特征。方法: 纳入北京大学口腔医院正畸科初诊拍摄大视野锥形束CT(cone-beam CT,CBCT)的11~14岁女性80例,按照上牙槽座点-鼻根点-下牙槽座点角(subspinale-nasion-supramental angle,ANB)和下颌平面角(Frankfort horizontal plane-gonion-gnathion angle,FH-GoGn)大小分为骨性Ⅰ类均角组(组1,0°≤ANB<4°,22°≤FH-GoGn≤32°),骨性Ⅱ类低角组(组2,ANB≥4°,FH-GoGn<22°)、均角组(组3,ANB≥4°,22°≤FH-GoGn≤32°)和高角组(组4,ANB≥4°,FH-GoGn>32°),每组20例,导入Dolphin软件进行头影测量和关节形态、位置测量。分别使用配对t检验、方差分析和卡方检验比较双侧关节对称性和关节形态及位置的组间差异,采用相关性分析探索骨性Ⅱ类人群头影测量值与关节测量项目间相关关系。结果: (1)关节对称性分析中,四组都存在少量差异有统计学意义的测量项目;组4双侧髁突位置不对称的样本量最多(65%), 其余三组比例相近,但差异无统计学意义。(2)对比组1和组3,关节形态学测量差异无统计学意义;髁突位置组1以前位和中位为主,组3居于后位者明显多于组1(χ2=6.936,P<0.05)。(3)在组2、3、4中,组2关节窝深度最深(H2&4=10.517,P=0.002),关节上间隙(LSD-t2&3=3.408,LSD-t2&4=5.369,P<0.001)、外间隙(LSD-t2&3=2.767,LSD-t2&4=3.350,P=0.001)最大;组4髁突长轴径最小(H2&4=13.374,P<0.001),关节窝垂直距最大(LSD-t2&4=4.561,P<0.001;LSD-t3&4=2.713,P=0.007),关节内间隙(LSD-t2&4=-4.083,P<0.001)、中间隙(LSD-t2&4=-4.201,P<0.001)最小。从组2、组3到组4,后位髁突所占比例逐渐升高。相关性分析显示,ANB与关节前间隙呈显著正相关(r=0.270,P=0.037),与髁突长轴角呈显著负相关(r=-0.296,P=0.022);FH-GoGn与关节上间隙(r=-0.488,P<0.001)、后间隙(r= -0.272,P=0.035)、内间隙(r=-0.390,P=0.002)、中间隙(r=-0.425,P=0.001)、外间隙(r=-0.331,P=0.010)、关节窝深度(r=-0.363,P=0.004)、关节结节后斜面倾斜度(r=-0.259,P=0.046)、髁突长轴径(r=-0.327,P=0.011)呈显著负相关,与关节窝垂直距呈显著正相关(r=0.370,P=0.004)。结论: Ⅱ类矢状骨面型的关节特征主要体现在髁突位置而非关节形态。Ⅱ类不同垂直骨面型关节形态及位置的差异更多地体现在关节间隙以及髁突和关节窝位置,从低角到高角关节窝位置逐渐增高,髁突后位比例逐渐增大。Ⅱ类高角的关节窝位置最高,髁突后位比例最大,关节间隙最小,关节窝深度最浅,髁突长轴径最短,关节不稳定因素最多,在进行正畸治疗时要尤其注意。
中图分类号:
- R783.5
| [1] |
Bjork A. Facial growth in man, studied with the aid of metallic implants[J]. Acta Odontol Scand, 1955,13(1):9-34.
doi: 10.3109/00016355509028170 pmid: 14398173 |
| [2] |
Copray JC, Dibbets JM, Kantomaa T. The role of condylar cartilage in the development of the temporomandibular joint[J]. Angle Orthod, 1988,58(4):369-380.
pmid: 3061315 |
| [3] |
Weinberg LA. Correlation of temporomandibular dysfunction with radiographic findings[J]. J Prosthet Dent, 1972,28(5):519-539.
doi: 10.1016/0022-3913(72)90064-9 pmid: 4507574 |
| [4] |
Ahn SJ, Lee SJ, Kim TW. Orthodontic effects on dentofacial morphology in women with bilateral TMJ disk displacement[J]. Angle Orthod, 2007,77(2):288-295.
pmid: 17319764 |
| [5] |
McNamara JA Jr. Components of class Ⅱ malocclusion in children 8-10 years of age[J]. Angle Orthod, 1981,51(3):177-202.
doi: 10.1043/0003-3219(1981)051<0177:COCIMI>2.0.CO;2 pmid: 7023290 |
| [6] |
Simmons 3rd HC, Oxford DE, Hill MD. The prevalence of skeletal Class Ⅱ patients found in a consecutive population presenting for TMD treatment compared to the national average[J]. J Tenn Dent Assoc, 2008,88(4):16-18.
pmid: 19248341 |
| [7] | Lin M, Xu Y, Wu H, et al. Comparative cone-beam computed tomography evaluation of temporomandibular joint position and morphology in female patients with skeletal class Ⅱ malocclusion[J]. J Int Med Res, 2019,48(2):0300060519892388. |
| [8] |
Hasebe A, Yamaguchi T, Nakawaki T, et al. Comparison of condylar size among different anteroposterior and vertical skeletal patterns using cone-beam computed tomography[J]. Angle Orthod, 2019,89(2):306-311.
doi: 10.2319/032518-229.1 pmid: 30475648 |
| [9] |
Ma Q, Bimal P, Mei L, et al. Temporomandibular condylar morphology in diverse maxillary-mandibular skeletal patterns: A 3-dimensional cone-beam computed tomography study[J]. J Am Dent Assoc, 2018,149(7):589-598.
doi: 10.1016/j.adaj.2018.02.016 pmid: 29655707 |
| [10] |
Pullinger A, Hollender L. Variation in condyle-fossa relationships according to different methods of evaluation in tomograms[J]. Oral Surg Oral Med Oral Pathol, 1986,62(6):719-727.
doi: 10.1016/0030-4220(86)90270-7 pmid: 3467295 |
| [11] | Ocak M, Sargon MF, Orhan K, et al. Evaluation of the anatomical measurements of the temporomandibular joint by cone-beam computed tomography[J]. Folia Morphol, 2019,78(1):174-181. |
| [12] |
Tsiklakis K, Syriopoulos K, Stamatakis HC. Radiographic examination of the temporomandibular joint using cone beam computed tomography[J]. Dentomaxillofac Radiol, 2004,33(3):196-201.
doi: 10.1259/dmfr/27403192 pmid: 15371321 |
| [13] |
Firetto MC, Abbinante A, Barbato E, et al. National guidelines for dental diagnostic imaging in the developmental age[J]. Radiol Med, 2019,124(9):887-916.
doi: 10.1007/s11547-019-01038-4 pmid: 31055724 |
| [14] | Bjork A. Variations in the growth pattern of the human mandible: Longitudinal radiographic study by the implant method[J]. J Dent Res, 1963,42(1):400-411. |
| [15] |
Lobo F, Tolentino ES, Iwaki LCV, et al. Imaginology tridimensional study of temporomandibular joint osseous components according to sagittal skeletal relationship, sex, and age[J]. J Craniofac Surg, 2019,30(5):1462-1465.
doi: 10.1097/SCS.0000000000005467 pmid: 31299744 |
| [16] |
Al-koshab M, Nambiar P, John J. Assessment of condyle and glenoid fossa morphology using CBCT in South-East Asians[J]. PLoS One, 2015,10(3):e0121682.
doi: 10.1371/journal.pone.0121682 pmid: 25803868 |
| [17] |
Coombs MC, She X, Brown T R, et al. Temporomandibular joint condyle-disc morphometric sexual dimorphisms independent of skull scaling[J]. J Oral Maxillofac Surg, 2019,77(11):2245-2257.
doi: 10.1016/j.joms.2019.04.022 pmid: 31125537 |
| [18] |
Weinberg LA. Role of condylar position in TMJ dysfunction-pain syndrome[J]. J Prosthet Dent, 1979,41(6):636-643.
doi: 10.1016/0022-3913(79)90062-3 pmid: 286056 |
| [19] | 葛胜将. 不同骨性错牙合患者髁突形态及位置的CBCT研究[D]. 青岛: 青岛大学, 2015. |
| [20] | 韩晓利. 成年女性骨性Ⅱ错牙合不同垂直骨面型患者TMJ骨性结构特征的CBCT研究[D]. 天津: 天津医科大学, 2017. |
| [21] | 崔燕, 唐天琪, 刘琳. 不同矢状骨面型患者颞下颌关节形态特征锥形束CT研究[J]. 中国实用口腔科杂志, 2016,9(6):348-353. |
| [22] |
Saccucci M, Polimeni A, Festa F, et al. Do skeletal cephalometric characteristics correlate with condylar volume, surface and shape? A 3D analysis[J]. Head Face Med, 2012,8:15.
doi: 10.1186/1746-160X-8-15 pmid: 22587445 |
| [23] |
Katayama K, Yamaguchi T, Sugiura M, et al. Evaluation of mandibular volume using cone-beam computed tomography and correlation with cephalometric values[J]. Angle Orthod, 2014,84(2):337-342.
doi: 10.2319/012913-87.1 pmid: 23985034 |
| [24] |
Paknahad M, Shahidi S, Abbaszade H. Correlation between condylar position and different sagittal skeletal facial types[J]. J Orofac Orthop, 2016,77(5):350-356.
doi: 10.1007/s00056-016-0039-z pmid: 27357584 |
| [25] |
Nielsen IL. Vertical malocclusions: etiology, development, diagnosis and some aspects of treatment[J]. Angle Orthod, 1991,61(4):247-260.
doi: 10.1043/0003-3219(1991)061<0247:VMEDDA>2.0.CO;2 pmid: 1763835 |
| [26] |
Droel R, Isaacson RJ. Some relationships between the glenoid fossa position and various skeletal discrepancies[J]. Am J Orthod, 1972,61(1):64-78.
doi: 10.1016/0002-9416(72)90177-7 pmid: 4500188 |
| [27] |
Costa EDD, Peyneau PD, Roque-Torres GD, et al. The relationship of articular eminence and mandibular fossa morphology to facial profile and gender determined by cone beam computed tomography[J]. Oral Surg Oral Med Oral Pathol Oral Radiol, 2019,128(6):660-666.
doi: 10.1016/j.oooo.2019.07.007 pmid: 31494114 |
| [28] |
Kurusu A, Horiuchi M, Soma K. Relationship between occlusal force and mandibular condyle morphology. Evaluated by limited cone-beam computed tomography[J]. Angle Orthod, 2009,79(6):1063-1069.
doi: 10.2319/120908-620R.1 pmid: 19852595 |
| [29] |
Burke G, Major P, Glover K, et al. Correlations between condylar characteristics and facial morphology in Class Ⅱ preadolescent patients[J]. Am J Orthod Dentofacial Orthop, 1998,114(3):328-336.
doi: 10.1016/s0889-5406(98)70216-1 pmid: 9743139 |
| [30] | 李晨. 不同垂直骨面型骨性Ⅱ类成年女性颞下颌关节骨性结构的三维分析[D]. 西安: 第四军医大学, 2016. |
| [31] |
Goymen M, Gulec A. Effects of the vertical malocclusion types on the dimension of the mandibular condyle[J]. Turk J Orthod, 2017,30(4):106-109.
doi: 10.5152/TurkJOrthod.2017.17029 pmid: 30112501 |
| [32] | 车蓓, 张昊, 钱才梅, 等. 不同垂直骨面型安氏Ⅱ类1分类错牙合患者颞下颌关节三维形态结构的比较[J]. 中华口腔医学杂志, 2014,49(7):399-402. |
| [33] |
Celik S, Celikoglu M, Buyuk SK, et al. Mandibular vertical asymmetry in adult orthodontic patients with different vertical growth patterns: A cone beam computed tomography study[J]. Angle Orthod, 2016,86(2):271-277.
doi: 10.2319/030515-135.1 pmid: 26065465 |
| [34] |
Kikuchi K, Takeuchi S, Tanaka E, et al. Association between condylar position, joint morphology and craniofacial morphology in orthodontic patients without temporomandibular joint disorders[J]. J Oral Rehabil, 2003,30(11):1070-1075.
doi: 10.1046/j.1365-2842.2003.01194.x pmid: 14641670 |
| [35] |
Paknahad M, Shahidi S. Association between condylar position and vertical skeletal craniofacial morphology: a cone beam computed tomography study[J]. Int Orthod, 2017,15(4):740-751.
doi: 10.1016/j.ortho.2017.09.008 pmid: 29111128 |
| [36] |
Park IY, Kim JH, Park YH. Three-dimensional cone-beam computed tomography based comparison of condylar position and morphology according to the vertical skeletal pattern[J]. Korean J Orthod, 2015,45(2):66-73.
doi: 10.4041/kjod.2015.45.2.66 pmid: 25798412 |
| [1] | 王敏, 李倩. 青少年抑郁症患者心理弹性影响因素的路径分析[J]. 北京大学学报(医学版), 2024, 56(5): 809-814. |
| [2] | 沈鹤军,侍崇艳,郑清,黄玉,景涛. 我国高中生静坐时长与健康素养现状及其影响因素调查[J]. 北京大学学报(医学版), 2024, 56(2): 239-246. |
| [3] | 李红光,韩玮华,吴训,冯继玲,李刚,孟娟红. 关节腔冲洗联合液态浓缩生长因子注射治疗单侧颞下颌关节骨关节炎的初步研究[J]. 北京大学学报(医学版), 2024, 56(2): 338-344. |
| [4] | 毛渤淳,田雅婧,王雪东,李晶,周彦恒. 骨性Ⅱ类高角患者拔牙矫治前后的面部软硬组织变化[J]. 北京大学学报(医学版), 2024, 56(1): 111-119. |
| [5] | 崔孟杰,马奇,陈曼曼,马涛,王鑫鑫,刘婕妤,张奕,陈力,蒋家诺,袁雯,郭桐君,董彦会,马军,星一. 不同生长模式与7~17岁儿童青少年代谢综合征的关系[J]. 北京大学学报(医学版), 2023, 55(3): 415-420. |
| [6] | 党佳佳,蔡珊,钟盼亮,王雅琪,刘云飞,师嫡,陈子玥,张依航,胡佩瑾,李晶,马军,宋逸. 室外夜间人工光暴露与中国9~18岁儿童青少年超重肥胖的关联[J]. 北京大学学报(医学版), 2023, 55(3): 421-428. |
| [7] | 郑丹枫,李君禹,李佳曦,张英爽,钟延丰,于淼. 青少年特发性脊柱侧凸椎旁肌的病理特征[J]. 北京大学学报(医学版), 2023, 55(2): 283-291. |
| [8] | 付玉,胡鑫浓,崔圣洁,施捷. 骨性Ⅱ类高角错 |
| [9] | 刘云飞,党佳佳,钟盼亮,马宁,师嫡,宋逸. 1990—2019年中国5~24岁人群伤害死亡率分析[J]. 北京大学学报(医学版), 2022, 54(3): 498-504. |
| [10] | 陈曼曼,杨招庚,苏彬彬,李艳辉,高迪,马莹,马涛,董彦会,马军. 中山市儿童青少年青春期身高生长突增规律[J]. 北京大学学报(医学版), 2021, 53(3): 506-510. |
| [11] | 杨雪,孙伟,王哲,姬爱平,白洁. 儿童和青少年牙外伤急诊患者临床分析[J]. 北京大学学报(医学版), 2021, 53(2): 384-389. |
| [12] | 韩玮华,罗海燕,郭传瑸,宁琦,孟娟红. 软骨寡聚基质蛋白在颞下颌关节滑膜软骨瘤病中的表达[J]. 北京大学学报(医学版), 2021, 53(1): 34-39. |
| [13] | 罗冬梅,闫晓晋,胡佩瑾,张京舒,宋逸,马军. 1990—2010年中国女性早婚和生育的地区不平等性[J]. 北京大学学报(医学版), 2020, 52(3): 479-485. |
| [14] | 陈硕,贺洋,安金刚,张益. 计算机辅助设计虚拟颌位在儿童颞下颌关节强直合并颌骨畸形同期矫治中的应用[J]. 北京大学学报(医学版), 2019, 51(5): 954-958. |
| [15] | 陶春燕,李红霞,李雪迎,唐朝枢,金红芳,杜军保. 体位性心动过速综合征儿童及青少年在直立试验中血流动力学变化[J]. 北京大学学报(医学版), 2019, 51(3): 414-421. |
|
||