北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 946-951. doi: 10.19723/j.issn.1671-167X.2021.05.023
全身麻醉下小儿开颅术术中心脏前负荷动态指标的一致性分析
- 北京大学第一医院1. 麻醉科, 北京 100034
2.儿童癫痫中心, 北京 100034
Comparison of pulse pressure variation, stroke volume variation, and plethysmographic variability index in pediatric patients undergoing craniotomy
LIU Ya-fei1,SONG Lin-lin1,△( ),XING Mao-wei1,CAI Li-xin2,WANG Dong-xin1
),XING Mao-wei1,CAI Li-xin2,WANG Dong-xin1
- 1. Department of Anesthesiology, Beijing 100034, China
2. Pediatric Epilepsy Center, Peking University First Hospital, Beijing 100034, China
摘要:
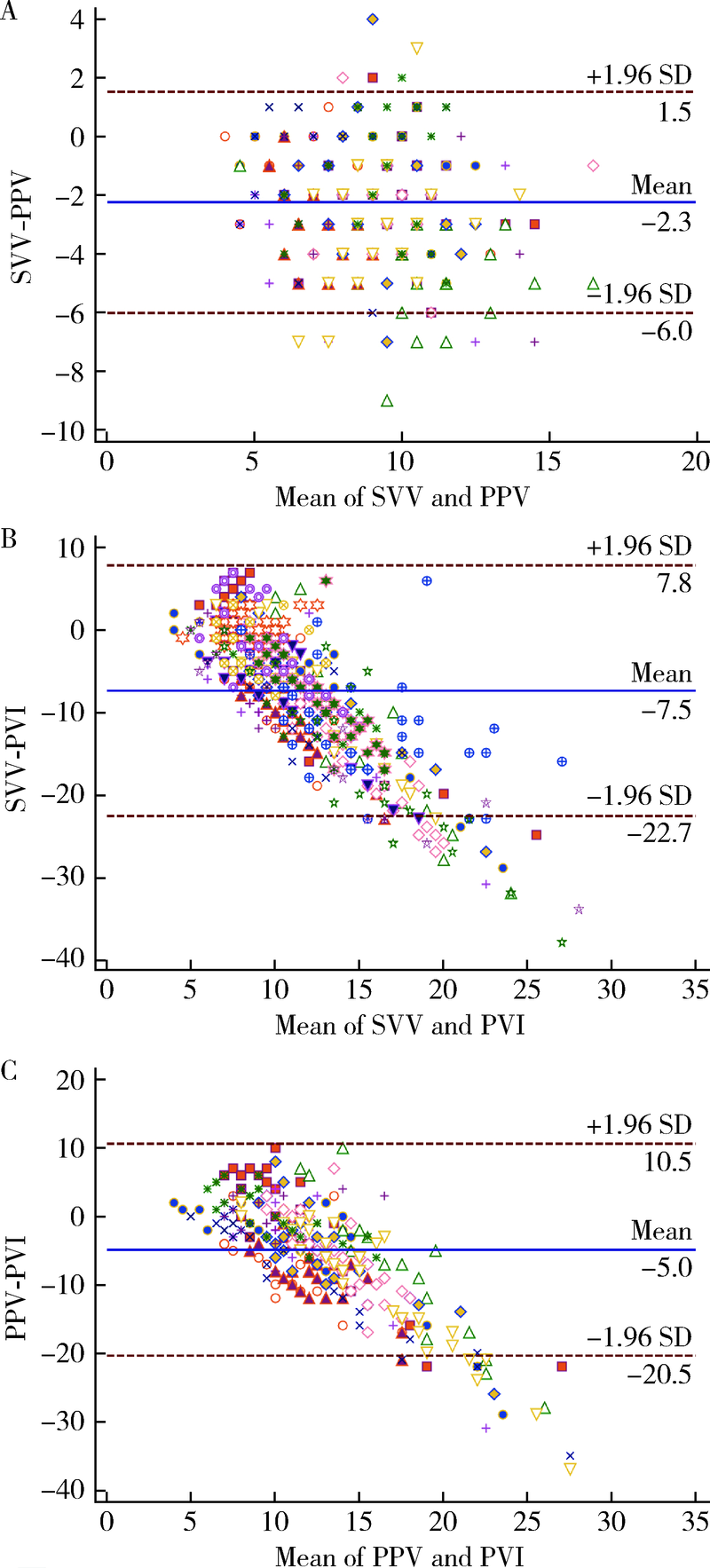
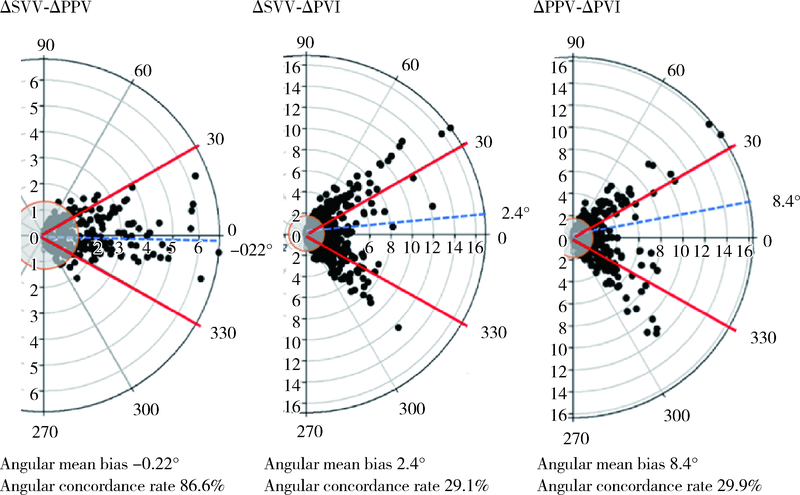
目的: 在小儿开颅癫痫病灶切除术中连续监测每搏量变异(stroke volume variation, SVV)、脉压变异(pulse pressure variation, PPV)和脉搏容积变异(plethysmographic variability index, PVI)3项心脏前负荷动态指标,评价这些常用动态指标的一致性,探索三者之间是否可以互换,以简化临床决策过程。方法: 30例行择期开颅癫痫病灶切除术的0 ~ 14岁患儿术中常规监测SVV、PPV和PVI, 根据上述指标和动脉收缩压实施目标导向液体管理。所有数据对分为6个阶段,每个阶段选取3 ~ 8个数据对,用Bland-Altman法分析数据对数值的一致性,用四象限图和极图分析数据对的同向变化趋势。结果: 患儿术中动脉收缩压为 (94±19) mmHg,平均SVV、PPV和PVI分别为8%±2%、10%±3%和15%±7%,共分析834个数据对。Bland-Altman分析显示SVV-PPV的平均偏倚为-2.3,一致限为-6.0 ~ 1.5,误差百分比为26%。SVV-PVI和PPV-PVI的平均偏倚分别为-7.5和-5.0,一致限分别为-22.7 ~ 7.8和-20.5 ~ 10.5,误差百分比分别为54%和43%。四象限图分析中3项指标变化的符合率分别为ΔSVV-ΔPPV 88.6%、ΔSVV-ΔPVI 50.1%、ΔPPV-ΔPVI 50.4%。<3岁者PPV-SVV符合率高于≥ 3岁者(92.7%与84.2%)。极坐标图分析中SVV-PPV变化的角符合率为86.6%,基于动脉压力波形的指标(SVV和PPV)与PVI变化符合率较差(分别为29.1%和29.9%)。结论: 小儿开颅术中SVV和PPV变化趋势一致性较高,尤其<3岁者,二者可以互换,无需额外使用SVV监测设备;但基于动脉压力波形的指标(SVV和PPV)与PVI之间变化趋势的一致性较差,不能互换。联合PPV和PVI用于监测心脏前负荷可能有助于提高小儿术中补液反应性的预测值。
中图分类号:
- R726.1
| [1] |
Chen PH, Chan KC, Liao MH, et al. Accuracy of dynamic preload variables for predicting fluid responsiveness in patients with pediatric liver cirrhosis: a prospective study [J]. Paediatr Anaesth, 2020, 30(4):455-461.
doi: 10.1111/pan.v30.4 |
| [2] |
Cheng YW, Xu F, Li J. Identification of volume parameters monitored with a noninvasive ultrasonic cardiac output monitor for predicting fluid responsiveness in children after congenital heart disease surgery [J]. Medicine (Baltimore), 2018, 97(39):e12289.
doi: 10.1097/MD.0000000000012289 |
| [3] |
Liu T, Xu C, Wang M, et al. Reliability of pleth variability index in predicting preload responsiveness of mechanically ventilated patients under various conditions: a systematic review and meta-analysis [J]. BMC Anesthesiol, 2019, 19(1):67.
doi: 10.1186/s12871-019-0744-4 |
| [4] |
Kim DH, Shin S, Kim JY, et al. Pulse pressure variation and pleth variability index as predictors of fluid responsiveness in patients undergoing spinal surgery in the prone position [J]. Ther Clin Risk Manag, 2018, 14:1175-1183.
doi: 10.2147/TCRM |
| [5] |
Saugel B, Heeschen J, Hapfelmeier A, et al. Cardiac output estimation using multi-beat analysis of the radial arterial blood pressure waveform: a method comparison study in patients having off-pump coronary artery bypass surgery using intermittent pulmonary artery thermodilution as the reference method [J]. J Clin Monit Comput, 2020, 34(4):649-654.
doi: 10.1007/s10877-019-00375-z pmid: 31456072 |
| [6] | Monnet X, Marik PE, Teboul JL. Prediction of fluid responsiveness: an update [J]. Ann Intensive Care, 2016, 2016(6):111. |
| [7] |
Joosten A, Jacobs A, Desebbe O, et al. Monitoring of pulse pressure variation using a new smartphone application (Capstesia) versus stroke volume variation using an uncalibrated pulse wave analysis monitor: a clinical decision making study during major abdominal surgery [J]. J Clin Monit Comput, 2019, 33(5):787-793.
doi: 10.1007/s10877-018-00241-4 |
| [8] |
Ji SH, Song IK, Jang YE, et al. Comparison of pulse pressure variation and pleth variability index in the prone position in pediatric patients under 2 years old [J]. Korean J Anesthesiol, 2019, 72(5):466-471.
doi: 10.4097/kja.19128 |
| [9] |
Desgranges FP, Evain JN, Pereira de Souza NE, et al. Does the plethysmographic variability index predict fluid responsiveness in mechanically ventilated children? A meta-analysis [J]. Br J Anaesth, 2016, 117(3):409-410.
doi: 10.1093/bja/aew245 pmid: 27543550 |
| [10] |
Lee JH, Kim EH, Jang YE, et al. Fluid responsiveness in the pediatric population [J]. Korean J Anesthesiol, 2019, 72(5):429-440.
doi: 10.4097/kja.19305 |
| [1] | 赵双云, 邹思雨, 李雪莹, 沈丽娟, 周虹. 中文版口腔健康素养量表简版(HeLD-14)在学龄前儿童家长中应用的信度和效度评价[J]. 北京大学学报(医学版), 2024, 56(5): 828-832. |
| [2] | 陈心心, 唐哲, 乔艳春, 荣文笙. 北京市密云区4岁儿童患龋状况及其与龋活跃性检测的相关性[J]. 北京大学学报(医学版), 2024, 56(5): 833-838. |
| [3] | 岳芷涵,韩娜,鲍筝,吕瑾莨,周天一,计岳龙,王辉,刘珏,王海俊. 儿童早期体重指数轨迹与超重风险关联的前瞻性队列研究[J]. 北京大学学报(医学版), 2024, 56(3): 390-396. |
| [4] | 费秀文,刘斯,汪波,董爱梅. 成人及儿童组织坏死性淋巴结炎临床特征及治疗[J]. 北京大学学报(医学版), 2024, 56(3): 533-540. |
| [5] | 俞光岩. 儿童唾液腺疾病[J]. 北京大学学报(医学版), 2024, 56(1): 1-3. |
| [6] | 闫晓晋,刘云飞,马宁,党佳佳,张京舒,钟盼亮,胡佩瑾,宋逸,马军. 《中国儿童发展纲要(2011-2020年)》实施期间中小学生营养不良率变化及其政策效应分析[J]. 北京大学学报(医学版), 2023, 55(4): 593-599. |
| [7] | 弭小艺,侯杉杉,付子苑,周末,李昕璇,孟召学,蒋华芳,周虹. 中文版童年不良经历问卷在学龄前儿童父母中应用的信效度评价[J]. 北京大学学报(医学版), 2023, 55(3): 408-414. |
| [8] | 崔孟杰,马奇,陈曼曼,马涛,王鑫鑫,刘婕妤,张奕,陈力,蒋家诺,袁雯,郭桐君,董彦会,马军,星一. 不同生长模式与7~17岁儿童青少年代谢综合征的关系[J]. 北京大学学报(医学版), 2023, 55(3): 415-420. |
| [9] | 党佳佳,蔡珊,钟盼亮,王雅琪,刘云飞,师嫡,陈子玥,张依航,胡佩瑾,李晶,马军,宋逸. 室外夜间人工光暴露与中国9~18岁儿童青少年超重肥胖的关联[J]. 北京大学学报(医学版), 2023, 55(3): 421-428. |
| [10] | 陈敬,肖伍才,单蕊,宋洁云,刘峥. DRD2基因rs2587552多态性对儿童肥胖干预效果的影响:一项前瞻性、平行对照试验[J]. 北京大学学报(医学版), 2023, 55(3): 436-441. |
| [11] | 李辉,高阳旭,王书磊,姚红新. 恶性肿瘤患儿完全植入式静脉输液港手术并发症[J]. 北京大学学报(医学版), 2022, 54(6): 1167-1171. |
| [12] | 刘京,陆爱东,左英熹,吴珺,黄志卓,贾月萍,丁明明,张乐萍,秦炯. 儿童急性淋巴细胞白血病合并癫痫发作75例临床特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(5): 948-953. |
| [13] | 崔雅茜,杜军保,张清友,廖莹,刘平,王瑜丽,齐建光,闫辉,徐文瑞,刘雪芹,孙燕,孙楚凡,张春雨,陈永红,金红芳. 儿童直立不耐受和坐位不耐受的疾病谱及治疗方式十年回顾[J]. 北京大学学报(医学版), 2022, 54(5): 954-960. |
| [14] | 马涛,李艳辉,陈曼曼,马莹,高迪,陈力,马奇,张奕,刘婕妤,王鑫鑫,董彦会,马军. 青春期启动提前与儿童肥胖类型的关联研究: 基于横断面调查和队列调查[J]. 北京大学学报(医学版), 2022, 54(5): 961-970. |
| [15] | 杜燕燕,王健,贺兰,季丽娜,徐樨巍. 儿童川崎病合并轻微脑炎/脑病伴可逆性胼胝体压部病变综合征1例并文献复习[J]. 北京大学学报(医学版), 2022, 54(4): 756-761. |
|
||