北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 977-982. doi: 10.19723/j.issn.1671-167X.2021.05.028
比较两种改良式印章法辅助后牙树脂牙合贴面修复的形态准确性
- 北京大学口腔医学院·口腔医院,1.修复科, 北京 100081
2.技工中心 国家口腔医学中心 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室, 北京 100081
Morphology accuracy evaluation of direct composite occlusal veneer using two types of modified stamp-technique
YANG Yang1,PU Ting-ting2,CHEN Li1,TAN Jian-guo1,△( )
)
- 1. Department of Prosthodontics, Beijing 100081, China
2. Dental Laboratory, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology, Beijing 100081, China
摘要:
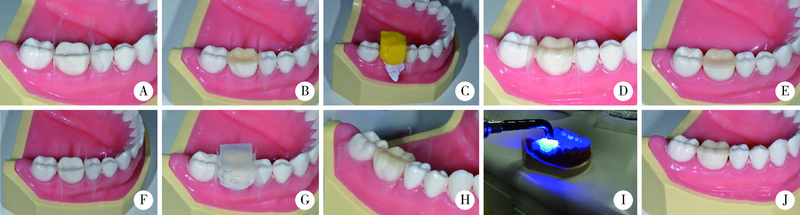
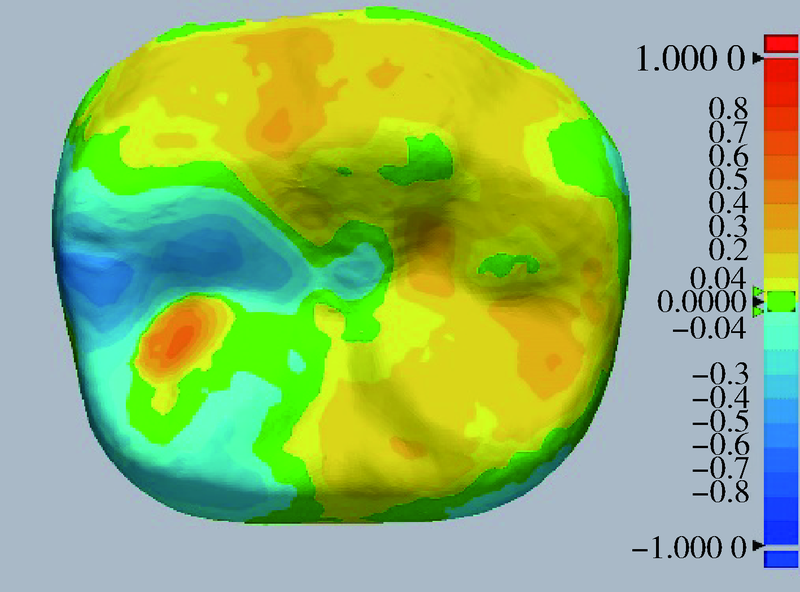
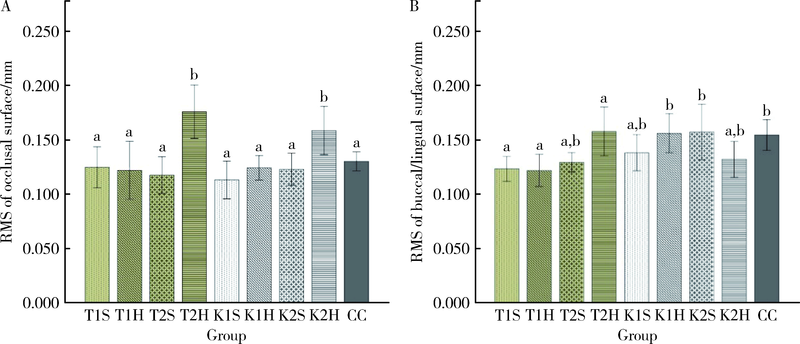
目的: 对比评价两种改良式印章法辅助后牙直接法复合树脂牙合贴面修复的形态准确性。方法: 采用标准树脂牙右下第一磨牙54颗,制作硬质硅橡胶和透明硅橡胶两种印章复制牙冠外形,并进行牙合贴面预备及复合树脂牙合贴面修复。试验共分为9组:按照不同印章(硬质硅橡胶或透明硅橡胶)、牙合面预备量(1 mm或2 mm)和不同复合树脂材料(通用型复合树脂或整块充填复合树脂)分为8个实验组,对照组为CAD/CAM生物复制方法进行间接修复。牙合贴面修复完成后进行模型扫描,并与修复前原始牙冠形态的扫描数据进行3D比较,按牙合面及轴面分别计算均方根(root mean square, RMS)值。采用方差分析比较各组RMS值。结果: 牙合面RMS值硬质硅橡胶印章法组为(0.136±0.031) mm,透明硅橡胶印章法组为(0.130±0.024) mm,对照组为(0.130±0.009) mm,组间差异无统计学意义;轴面RMS值分别为(0.135±0.020) mm、(0.147±0.021) mm及(0.153±0.014) mm,硬质硅橡胶印章法组最小(P<0.05)。两种改良式印章法在2 mm厚的通用型树脂组牙合面平均RMS值最大,显著大于对照组(P<0.05)。结论: 使用两种改良式印章法辅助进行直接法牙合贴面修复具有较高的形态准确性,硬质硅橡胶印章法所得修复体的轴面形态更佳。当修复体牙合面厚度为2 mm时,使用整块充填复合树脂具有更准确的牙合面形态。
中图分类号:
- R783
| [1] | 王晓燕, 岳林. 从复合树脂直接粘接修复材料的发展看临床技术指南 [J]. 中华口腔医学杂志, 2018, 53(6):374-380. |
| [2] |
Orgia E, Baron R, Borgia JL. Quality and survival of direct light-activated composite resin restorations in posterior teeth: a 5- to 20-year retrospective longitudinal study [J]. J Prosthodont, 2019, 28(1):e195-e203.
doi: 10.1111/jopr.12630 |
| [3] | Azeem RA, Sureshbabu NM. Clinical performance of direct versus indirect composite restorations in posterior teeth: a systematic review [J]. J Conserv Dent, 2018, 21(1):2-9. |
| [4] |
Attin T, Filli T, Imfeld C, et al. Composite vertical bite reconstructions in eroded dentitions after 5.5 years: a case series [J]. J Oral Rehabil, 2012, 39(1):73-79.
doi: 10.1111/j.1365-2842.2011.02240.x pmid: 21827523 |
| [5] |
Loomans B, Opdam N, Attin T, et al. Severe tooth wear: European consensus statement on anagement guidelines [J]. J Adhes Dent, 2017, 19(2):111-119.
doi: 10.3290/j.jad.a38102 pmid: 28439579 |
| [6] |
Alshehadat SA, Halim MS, Carmen K, et al. The stamp technique for direct Class II composite restorations: a case series [J]. J Conserv Dent, 2016, 19(5):490-493.
doi: 10.4103/0972-0707.190021 |
| [7] |
Ramseyer ST, Helbling C, Lussi A. Posterior ertical bite reconstructions of erosively worn dentitions and the “stamp technique”: a case series with a mean observation ime of 40 months [J]. J Adhes Dent, 2015, 17(3):283-289.
doi: 10.3290/j.jad.a34135 pmid: 26159125 |
| [8] |
Ammannato R, Ferraris F, Marchesi G. The “index technique” in worn dentition: a new and conservative approach [J]. Int J Esthet Dent, 2015, 10(1):68-99.
pmid: 25625128 |
| [9] |
Ammannato R, Rondoni D, Ferraris F. Update on the 'index technique’ in worn dentition: a no-prep restorative approach with a digital workflow [J]. Int J Esthet Dent, 2018, 13(4):516-537.
pmid: 30302440 |
| [10] |
Francisconi-Dos-Rios LF, Tavares JAO, Oliveira L, et al. Functional and aesthetic rehabilitation in posterior tooth with bulk-fill resin composite and occlusal matrix [J]. Restor Dent Endod, 2020, 45(1):e9.
doi: 10.5395/rde.2020.45.e9 |
| [11] |
Negrão R, Cardoso JA, de Oliveira NB, et al. Conservative restoration of the worn dentition: the anatomically driven direct approach (ADA) [J]. Int J Esthet Dent, 2018, 13(1):16-48.
pmid: 29379902 |
| [12] |
Milosevic A. Clinical guidance and an evidence-based approach for restoration of worn dentition by direct composite resin [J]. Br Dent J, 2018, 224(5):301-310.
doi: 10.1038/sj.bdj.2018.168 |
| [13] |
Hamburger JT, Opdam NJ, Bronkhorst EM, et al. Indirect restorations for severe tooth wear: fracture risk and layer thickness [J]. J Dent, 2014, 42(4):413-418.
doi: 10.1016/j.jdent.2013.10.003 pmid: 24120523 |
| [14] | 陈建洪, 徐雄均, 卢惠冰, 等. 三种材料修复老年人后牙重度磨损的疗效分析 [J]. 临床医学工程, 2013, 20(11):1351-1352. |
| [15] |
Wieckiewicz M, Grychowska N, Zietek M, et al. Evaluation of the elastic properties of thirteen silicone interocclusal recording materials [J]. Biomed Res Int, 2016, 2016:7456046.
pmid: 27747239 |
| [16] | 陈智, 张磊, 赵小娥. 大块充填树脂在牙体修复中的应用与研究进展 [J]. 口腔疾病防治, 2017, 25(4):205-209. |
| [17] | 张晓敏, 郑刚, 林红, 等. 十种纳米填料光固化复合树脂聚合收缩性能的比较与评价 [J]. 中华口腔医学杂志, 2013, 48(Suppl 1):120-124. |
| [18] |
Papadiochou S, Pissiotis AL. Marginal adaptation and CAD-CAM technology: a systematic review of restorative material and fabrication techniques [J]. J Prosthet Dent, 2018, 119(4):545-551.
doi: S0022-3913(17)30488-2 pmid: 28967399 |
| [19] | 李虹, 孙玉春, 赵一姣, 等. 三种牙颌模型扫描仪牙尖交错牙合三维重建精度评价 [J]. 口腔颌面修复学杂志, 2014, 15(2):65-69. |
| [1] | 李媛,林红,张铁军. 对比传统成像与数字成像对牙科复合树脂X射线阻射性的影响[J]. 北京大学学报(医学版), 2021, 53(5): 995-1001. |
| [2] | 穆海丽,田福聪,王晓燕,高学军. 玻璃体和通用型复合树脂耐磨性的临床对照研究[J]. 北京大学学报(医学版), 2021, 53(1): 120-125. |
| [3] | 于鹏,王晓燕. 填料折射率与比例对复合树脂折射率和透明度的影响[J]. 北京大学学报(医学版), 2020, 52(4): 790-793. |
| [4] | 唐仁韬,李欣海,于江利,冯琳,高学军. 复合树脂与玻璃陶瓷微拉伸粘接强度的体外研究[J]. 北京大学学报(医学版), 2020, 52(4): 755-761. |
| [5] | 李贝贝,邸萍. CAD/CAM钛合金表面处理工艺联合树脂粘接剂对硬质复合树脂粘接强度和耐久性的影响[J]. 北京大学学报(医学版), 2019, 51(1): 111-114. |
| [6] | 张皓羽,姜婷,程明轩,张玉玮. 类瓷树脂及玻璃陶瓷牙合贴面疲劳实验前后的磨耗及表面粗糙度的变化[J]. 北京大学学报(医学版), 2018, 50(1): 73-77. |
| [7] | 郭惠杰,高承志, 林斐,刘伟,岳林. 唾液污染对复合树脂间粘接强度的影响[J]. 北京大学学报(医学版), 2017, 49(1): 96-100. |
| [8] | 林斐, 刘伟, 闫鹏, 岳林. 复合树脂间粘接的微拉伸强度研究[J]. 北京大学学报(医学版), 2015, 47(1): 124-128. |
| [9] | 蔡雪, 聂杰, 王祖华, 田洪琰, 赵莹, 王晓燕. 洞缘形态对复合树脂颜色匹配的影响[J]. 北京大学学报(医学版), 2015, 47(1): 120-123. |
| [10] | 田福聪,王晓燕,高学军. 不同粘接系统用于楔状缺损直接修复的临床观察[J]. 北京大学学报(医学版), 2014, 46(1): 58-61. |
| [11] | 袁慎坡, 林红, 潘硕, 娄丽丽, 徐永祥. Polident义齿清洁剂对义齿基托树脂性能的影响[J]. 北京大学学报(医学版), 2012, 44(6): 946-949. |
| [12] | 徐永祥, 韩建民, 林红. 自黏性流动树脂的性能研究[J]. 北京大学学报(医学版), 2012, 44(2): 303-306. |
| [13] | 高博韬, 郑刚, 林红, 徐永祥. 实时动态分析牙科光固化复合树脂固化收缩的新方法[J]. 北京大学学报(医学版), 2011, 43(6): 895-899. |
| [14] | 韩冰, 董艳梅, 王晓燕, 高学军. 光照模式对复合树脂聚合收缩率和表面硬度的影响[J]. 北京大学学报(医学版), 2011, 43(5): 770-773. |
| [15] | 赵奇*, 薛世华*, 吴艳, 王世明. 应用龈色树脂修复前牙颈部缺损的临床评价[J]. 北京大学学报(医学版), 2011, 43(1): 44-47. |
|
||