北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (3): 537-544. doi: 10.19723/j.issn.1671-167X.2025.03.018
慢性阻塞性肺疾病患者体力活动与死亡风险的前瞻性关联
张烁1, 兰勇兵1, 孙点剑一1,2,3, 裴培2, 杜怀东4, 陈君石5, 陈铮鸣4, 吕筠1,2,3,6, 李立明1,2,3, 余灿清1,2,3,*( ), (代表中国慢性病前瞻性研究项目协作组)
), (代表中国慢性病前瞻性研究项目协作组)
- 1. 北京大学公共卫生学院流行病与卫生统计学系, 北京 100191
2. 北京大学公众健康与重大疫情防 控战略研究中心, 北京 100191
3. 重大疾病流行病学教育部重点实验室(北京大学), 北京 100191
4. Clinical Trial Service Unit and Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford OX3 7LF, UK
5. 国家食品安全风险评估中心, 北京 100022
6. 北京大学血管稳态与重构全国重点实验室, 北京 100191
Prospective association between physical activity and mortality in patients with chronic obstructive pulmonary disease
Shuo ZHANG1, Yongbing LAN1, Dianjianyi SUN1,2,3, Pei PEI2, Huaidong DU4, Junshi CHEN5, Zhengming CHEN4, Jun LV1,2,3,6, Liming LI1,2,3, Canqing YU1,2,3,*( ), (for the China Kadoorie Biobank Collaborative Group)
), (for the China Kadoorie Biobank Collaborative Group)
- 1. Department of Epidemiology & Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Peking University Center for Public Health and Epidemic Preparedness & Response, Beijing 100191, China
3. Key Laboratory of Epidemiology of Major Diseases (Peking University), Ministry of Education, Beijing 100191, China
4. Clinical Trial Service Unit and Epidemiological Studies Unit, Nuffield Department of Population Health, University of Oxford, Oxford OX3 7LF, UK
5. China National Center for Food Safety Risk Assessment, Beijing 100022, China
6. State Key Laboratory of Vascular Homeostasis and Remodeling, Peking University, Beijing 100191, China
摘要:
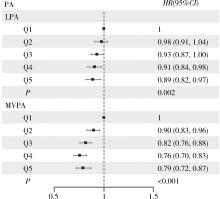
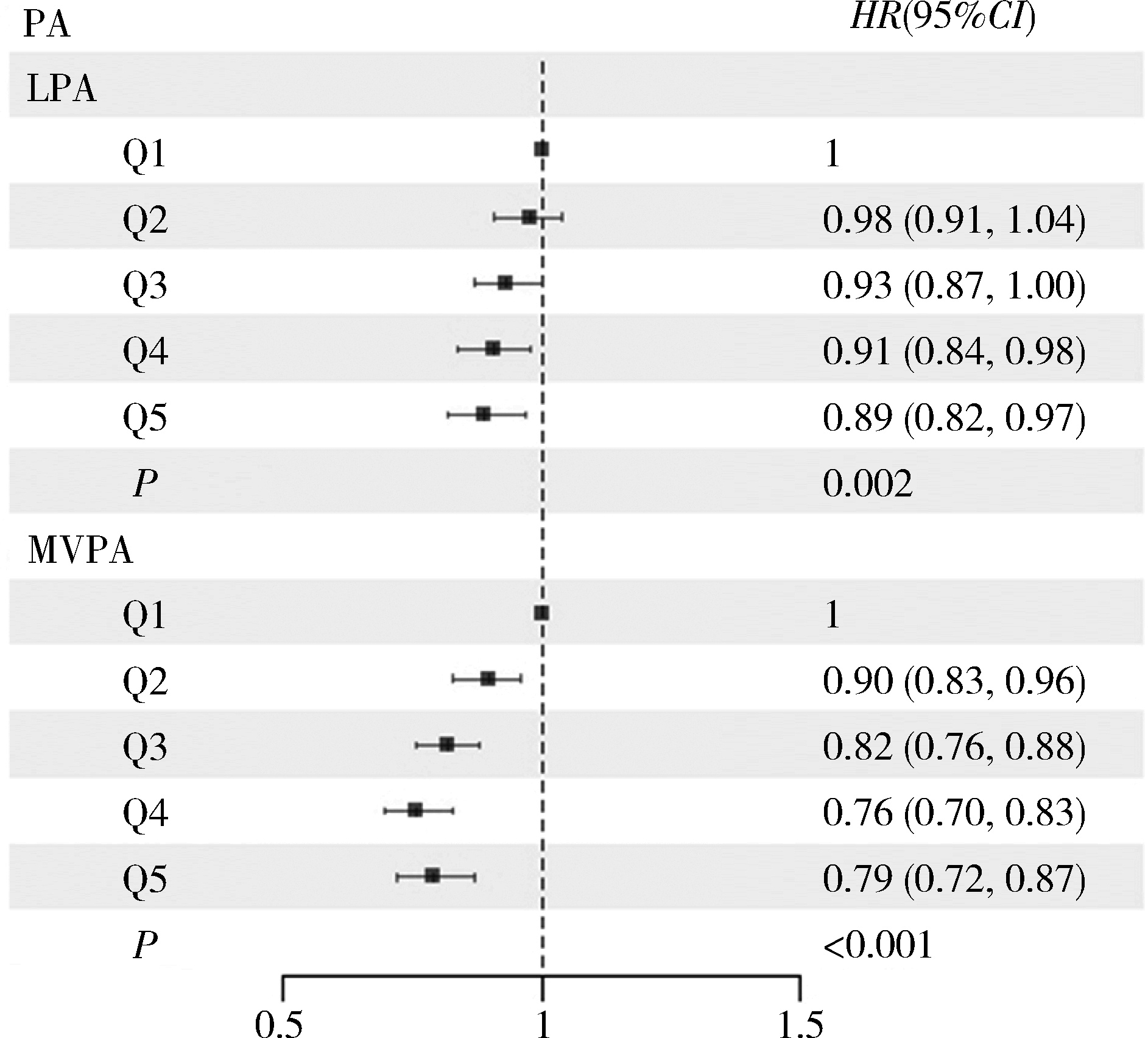
目的: 探讨中国成人慢性阻塞性肺疾病(chronic obstructive pulmonary disease, COPD)患者体力活动水平与死亡风险的前瞻性关联。方法: 基于中国慢性病前瞻性研究(China Kadoorie Biobank, CKB)项目, 采用Cox比例风险回归模型分析中国成人COPD患者中总体力活动、不同强度(低、中高强度)及不同类型(工作、非工作)体力活动水平与全因死亡、主要死因死亡风险的前瞻性关联, 根据体力活动水平的五分位数分为5组(Q1~Q5), 将体力活动水平最低五分位数组(Q1)作为对照组, 计算其余各组(Q2~Q5)风险比(hazard ratio, HR)及其95%置信区间(confidence interval, CI), 同时实施了敏感性分析及亚组分析, 包括年龄、性别、自评健康状况、COPD严重程度等。结果: 基线时纳入33 588例COPD患者, 平均随访(11.1±3.1)年, 共记录到死亡8 314人(22.3%)。总体力活动水平与全因死亡、血管疾病及呼吸系统疾病死亡风险之间存在线性负相关(线性趋势检验P值依次为 < 0.001、0.002、 < 0.001), 与总体力活动水平最低五分位数组(Q1)相比, 最高五分位数组(Q5)对应的全因死亡、血管疾病及呼吸系统疾病死亡风险HR值(95%CI)分别为0.77 (0.70, 0.85)、0.77 (0.65, 0.91)、0.58 (0.48, 0.71)。低强度、中高强度体力活动均与COPD患者全因死亡风险存在线性负相关关联(线性趋势检验P值依次为0.002、 < 0.001), 与低强度、中高强度体力活动水平最低五分位数组(Q1)相比, 最高五分位数组(Q5)全因死亡风险对应的HR值(95%CI)分别为0.89 (0.82, 0.97)、0.79 (0.72, 0.87)。工作、非工作相关体力活动亦与COPD患者全因死亡风险存在线性负相关关联(线性趋势检验P值依次为 < 0.001、0.015), 与工作、非工作相关体力活动水平最低五分位数组(Q1)相比, 最高五分位数组(Q5)全因死亡风险对应的HR值(95%CI)分别为0.69 (0.61, 0.78), 0.91 (0.84, 0.98)。对于年龄≥60岁、女性、自评健康状况较差的人群, 总体力活动与全因死亡风险负相关性更为显著。对于不同严重程度的COPD患者, 随着总体力活动的增加, 全因死亡风险均呈下降趋势。结论: 总体力活动、不同强度、不同类别的体力活动均与COPD患者的死亡风险呈负相关, 且存在剂量反应关系。对于年龄≥60岁、女性、自评健康状况较差的人群, 总体力活动与全因死亡风险负相关性更为显著。
中图分类号:
- R184
| 1 |
慢性阻塞性肺疾病急性加重诊治专家组. 慢性阻塞性肺疾病急性加重诊治中国专家共识[J]. 国际呼吸杂志, 2023, 43 (2): 132- 149.
|
| 2 |
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2025 update[EB/OL]. (2025-01-01)[2025-01-15]. https://www.goldcopd.org.
|
| 3 |
doi: 10.1016/S0140-6736(18)30841-9 |
| 4 |
doi: 10.1164/rccm.200612-1749OC |
| 5 |
doi: 10.1016/S2214-109X(23)00217-6 |
| 6 |
World Health Organization. WHO guidelines on physical activity and sedentary behaviour [EB/OL]. (2020-11-25)[2024-12-25]. https://www.who.int/publications/i/item/9789240015128.
|
| 7 |
doi: 10.1016/S0140-6736(17)31222-9 |
| 8 |
doi: 10.1093/ije/dyr120 |
| 9 |
doi: 10.1093/ije/dyi174 |
| 10 |
doi: 10.1249/MSS.0b013e31821ece12 |
| 11 |
樊萌语, 吕筠, 郭彧, 等. 中国慢性病前瞻性研究: 10个项目地区成人体力活动和休闲静坐时间特征差异的分析[J]. 中华流行病学杂志, 2015, 36 (8): 779- 785.
|
| 12 |
中华人民共和国国家卫生健康委员会医政司. 肥胖症诊疗指南(2024年版)[J]. 中华消化外科杂志, 2024, 23 (10): 1237- 1260.
doi: 10.3760/cma.j.cn115610-20241017-00455 |
| 13 |
doi: 10.1186/s12889-018-5167-5 |
| 14 |
孙明希, 温启邦, 涂华康, 等. 4种慢性病共病模式及运动与全因死亡的相关性研究[J]. 中华流行病学杂志, 2022, 43 (12): 1952- 1958.
|
| 15 |
doi: 10.1378/chest.10-2521 |
| 16 |
doi: 10.1378/chest.11-2014 |
| 17 |
doi: 10.1016/j.chest.2023.07.017 |
| 18 |
|
| 19 |
doi: 10.1097/PHM.0000000000002612 |
| 20 |
doi: 10.1080/17461391.2019.1697375 |
| 21 |
|
| 22 |
|
| 23 |
|
| 24 |
|
| 25 |
|
| 26 |
|
| 27 |
Hu YZ, Sun QF, Han YT, et al. Role of lifestyle factors on the development and long-term prognosis of pneumonia and cardiovascular disease in the Chinese population[J]. Chin Med J (Engl), 2024, 8 (2024-08-28)[2024-12-26]. https://pubmed.ncbi.nlm.nih.gov/39193696.
|
| [1] | 刘畅, 李炤, 金蕾, 刘春毅, 王春静, 张杰, 靳蕾. 母亲围受孕期服用叶酸营养素补充剂与围产儿死亡率的关系[J]. 北京大学学报(医学版), 2025, 57(3): 473-480. |
| [2] | 许秋实, 刘彤, 王俊杰. 铁死亡相关长链非编码核糖核酸预测放射治疗后非小细胞肺癌患者的临床结局[J]. 北京大学学报(医学版), 2025, 57(3): 569-577. |
| [3] | 赵柯林, 夏雪, 史乃旭, 周韩, 盖婧雯, 李萍. 铁死亡标志物4-HNE在系统性硬化症细胞模型中的表达及意义[J]. 北京大学学报(医学版), 2024, 56(6): 950-955. |
| [4] | 王裕新, 曹茹, 黄婧, Pitakchon Ponsawansong, Benjawan Tawatsupa, 潘小川, Tippawan Prapamontol, 李国星. 不同表观温度水平下大气细颗粒物暴露对人群非意外死亡的影响[J]. 北京大学学报(医学版), 2024, 56(5): 820-827. |
| [5] | 周庆欣,杨晴晴,石舒原,李沛,孙凤. 健康体检人群血尿酸与气流阻塞的相关性[J]. 北京大学学报(医学版), 2024, 56(4): 693-699. |
| [6] | 徐训敏,邵校,姬爱平. 口腔急诊科死亡病例分析[J]. 北京大学学报(医学版), 2024, 56(1): 185-189. |
| [7] | 王子恺,莫佳丽,张蒙,廖纪萍. 2013—2020年北京市慢性阻塞性肺疾病急性加重女性住院患者的流行病学和住院费用分析[J]. 北京大学学报(医学版), 2023, 55(6): 1074-1081. |
| [8] | 汪雨欣,邓宇含,谭银亮,刘宝花. 应激性血糖升高对重症监护病房患者28 d全因死亡风险的预测价值[J]. 北京大学学报(医学版), 2023, 55(3): 442-449. |
| [9] | 李东,邸吉廷,熊焰. 程序性细胞死亡1-配体1在不同免疫组织化学染色方法的一致性比较[J]. 北京大学学报(医学版), 2023, 55(2): 339-342. |
| [10] | 熊焰,张波,聂立功,吴世凯,赵虎,李东,邸吉廷. 胸部SMARCA4缺失性未分化肿瘤的病理诊断与联合免疫检测点抑制剂治疗[J]. 北京大学学报(医学版), 2023, 55(2): 351-356. |
| [11] | 赵亚楠,范慧芸,王翔宇,罗雅楠,张嵘,郑晓瑛. 孤独症患者过早死亡风险及死亡原因[J]. 北京大学学报(医学版), 2023, 55(2): 375-383. |
| [12] | 刘云飞,党佳佳,钟盼亮,马宁,师嫡,宋逸. 1990—2019年中国5~24岁人群伤害死亡率分析[J]. 北京大学学报(医学版), 2022, 54(3): 498-504. |
| [13] | 刘杰,郭超. 正/负性情绪对中国老年人死亡风险影响的前瞻性队列研究[J]. 北京大学学报(医学版), 2022, 54(2): 255-260. |
| [14] | 顾阳春,刘颖,谢超,曹宝山. 程序性死亡蛋白-1抑制剂治疗晚期肺癌出现垂体免疫不良反应3例[J]. 北京大学学报(医学版), 2022, 54(2): 369-375. |
| [15] | 包海荣,刘晓菊,谭恩丽,舒娟,董继元,李盛. 兰州市气温和相对湿度对慢性阻塞性肺疾病患者门诊就诊人次的影响及其交互效应[J]. 北京大学学报(医学版), 2020, 52(2): 308-316. |
|
||