北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (5): 802-811. doi: 10.19723/j.issn.1671-167X.2023.05.005
青年肾肿瘤伴瘤栓的临床病理特征及预后分析
薛子璇1,唐世英1,邱敏1,*( ),刘承2,*(
),刘承2,*( ),田晓军1,陆敏3,董靖晗1,马潞林1,张树栋1
),田晓军1,陆敏3,董靖晗1,马潞林1,张树栋1
- 1. 北京大学第三医院泌尿外科,北京 100191
2. 上海市第一人民医院泌尿外科,上海 200940
3. 北京大学第三医院病理科,北京 100191
Clinicopathologic features and prognosis of young renal tumors with tumor thrombus
Zi-xuan XUE1,Shi-ying TANG1,Min QIU1,*( ),Cheng LIU2,*(
),Cheng LIU2,*( ),Xiao-jun TIAN1,Min LU3,Jing-han DONG1,Lu-lin MA1,Shu-dong ZHANG1
),Xiao-jun TIAN1,Min LU3,Jing-han DONG1,Lu-lin MA1,Shu-dong ZHANG1
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Urology, Shanghai First People' s Hospital, Shanghai 200940, China
3. Department of Pathology, Peking University Third Hospital, Beijing 100191, China
摘要:
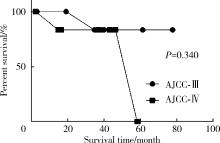
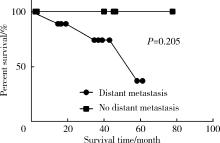
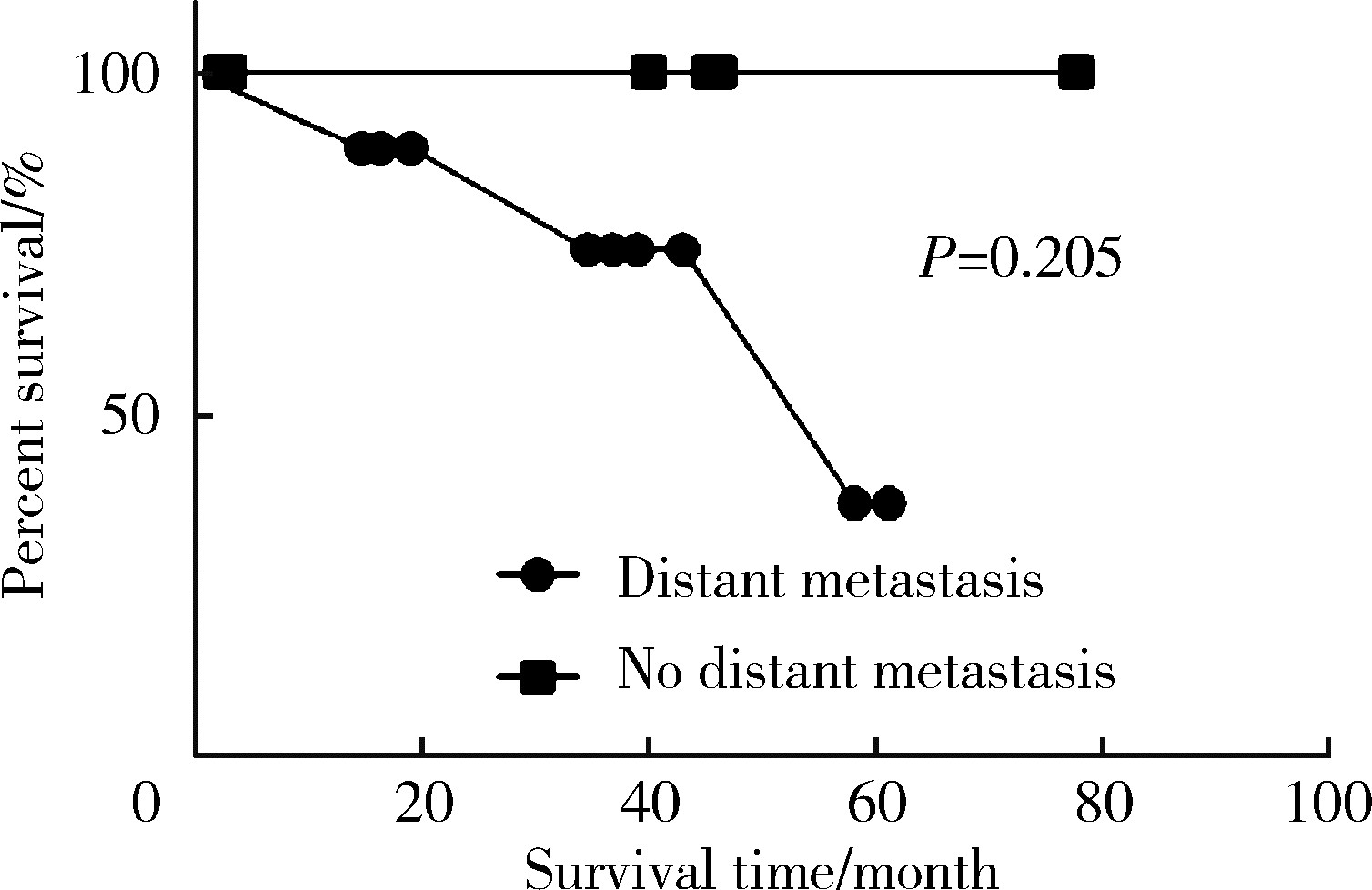
目的: 回顾性分析2016年1月至2022年12月于北京大学第三医院因肾肿瘤伴瘤栓行手术治疗的患者(年龄≤40岁)临床资料,评估手术效果,探讨其临床病理特征与预后之间的关系。方法: 回顾17例青年肾肿瘤伴瘤栓患者的临床资料,总结其临床病理特征和预后情况。按照有无症状、2017年美国癌症联合委员会(American Joint Committee on Cancer, AJCC)的临床分期、术后有无联合辅助治疗进行分组,采用Kaplan-Meier方法描绘生存曲线,并采用Log-rank检验比较不同组间患者术后生存时间、无进展生存时间的差异,分析临床病理特征和预后的关系。结果: 17例患者均接受静脉瘤栓取出术,其中,肾根治性切除术16例(94.1%),保留肾单位术1例(5.9%);术前有症状者12例(70.6%),无症状者5例(29.4%);良性肾肿瘤2例(11.8%),恶性肾肿瘤15例(88.2%),包括肾透明细胞癌1例(6.7%),非透明细胞癌14例(93.3%)。15例恶性肾肿瘤中,AJCC临床Ⅲ期8例(53.3%),Ⅳ期7例(46.7%)。术后联合多种辅助治疗者6例(40%),未联合多种辅助治疗者9例(60%)。随访时间2~78个月,中位随访时间41个月,随访中死亡3例(20%)。患者术后中位生存时间39.0 (2.3,77.8)个月,无进展生存时间16.4 (2.3,77.8)个月。根据术前有无症状(P=0.307,P=0.302)、AJCC临床分期(P=0.340,P=0.492)、术后有无联合辅助治疗(P=0.459,P=0.253)分组,青年肾肿瘤伴瘤栓患者的术后生存时间、无进展生存时间差异无统计学意义。结论: 青年肾肿瘤伴瘤栓患者多出现症状,病理类型更复杂多样,恶性肿瘤合并瘤栓中非透明细胞癌的比例更高,有症状及非透明细胞癌与不良预后可能存在一定潜在相关性,外科手术联合辅助治疗是青年肾肿瘤伴瘤栓患者相对安全、有效的治疗方式。
中图分类号:
- R737.11
| 1 |
BukavinaL , BensalahK , BrayF ,et al.Epidemiology of renal cell carcinoma: 2022 update[J].Eur Urol,2022,82(5):529-542.
doi: 10.1016/j.eururo.2022.08.019 |
| 2 | 南宁.青年肾肿瘤的临床特点及预后分析[J].中外医疗,2016,35(10):87-89. |
| 3 | 刘俊杰, 刘子颉, 夏斌,等.肾肿瘤伴静脉瘤栓患者的手术疗效及相关预后因素分析[J].徐州医科大学学报,2021,41(6):399-402. |
| 4 | 王海, 张瑞强, 王清海,等.青年肾细胞癌临床病理特点及预后分析[J].北京医学,2013,35(10):844-846. |
| 5 | 龙嘉辉. 机器人辅助腹腔镜手术治疗肾肿瘤伴静脉瘤栓的临床研究[D]. 南昌: 南昌大学, 2022. |
| 6 |
JuradoA , RomeoA , GueglioG ,et al.Current trends in management of renal cell carcinoma with venous thrombus extension[J].Curr Urol Rep,2021,22(4):23.
doi: 10.1007/s11934-021-01036-y |
| 7 | 徐之鹏, 李青楠, 董喆,等.青年肾肿瘤的临床特点分析[J].中国医科大学学报,2013,42(9):852-854. |
| 8 |
PatardJJ .Incidental renal tumours[J].Curr Opin Urol,2009,19(5):454-458.
doi: 10.1097/MOU.0b013e32832f0ccd |
| 9 | 黄力, 陈从波, 姚启盛,等.肾错构瘤并肾静脉瘤栓1例[J].现代泌尿生殖肿瘤杂志,2020,12(6):365. |
| 10 | 杨斌, 邱敏, 卢剑,等.同期后腹腔镜肾盂离断成形术联合肾部分切除术的安全性观察[J].临床泌尿外科杂志,2017,32(8):639-641. |
| 11 | 邱敏, 田晓军, 卢剑,等.后腹腔镜肾部分切除术治疗巨大(≥8 cm)肾错构瘤的技巧探讨[J].中国微创外科杂志,2017,17(10):905-908. |
| 12 | 刘茁, 朱国栋, 唐世英,等.外科手术治疗年龄≥75岁的高龄肾细胞癌合并静脉癌栓患者的临床经验[J].北京大学学报(医学版),2022,54(4):774-778. |
| 13 | 黄子雄, 杜依青, 张晓鹏,等.肾细胞癌骨转移的临床与病理分析[J].北京大学学报(医学版),2018,50(5):811-815. |
| 14 | 王林辉. 青年肾细胞癌患者的临床病理特点及诊治分析[M]// 仲剑平. 中国外科年鉴. 上海: 第二军医大学出版社, 2012: 466. |
| 15 |
CapitanioU , BensalahK , BexA ,et al.Epidemiology of renal cell carcinoma[J].Eur Urol,2019,75(1):74-84.
doi: 10.1016/j.eururo.2018.08.036 |
| 16 | 储婧.儿童肾母细胞瘤临床病理资料与预后的影响因素分析[J].临床泌尿外科杂志,2023,38(4):260-264. |
| 17 | 洪博, 董瑞.肾母细胞瘤治疗研究进展[J].临床小儿外科杂志,2021,20(6):569-575. |
| 18 | 张崔建, 李学松, 虞巍,等.成人肾母细胞瘤的治疗及其长期随访结果[J].北京大学学报(医学版),2012,44(4):535-538. |
| 19 | 王亚楠, 田亚明, 许艳平,等.儿童肾母细胞瘤的临床病理特征及预后影响因素分析[J].实用癌症杂志,2022,37(4):653-655. |
| 20 | 盛琦, 张勤, 袁晓军, 等. 儿童晚期肾母细胞瘤的诊治[C]// 浙江省医学会. 2012年江浙沪儿科学术年会暨浙江省医学会儿科学分会学术年会暨儿内科疾病诊治新进展国家级学习班论文汇编. 浙江: [出版者不详], 2012: 153-154. |
| 21 | 博尔术, 洪鹏, 张宇,等.乳头状肾细胞癌的临床病理特征和预后分析[J].北京大学学报(医学版),2022,54(4):615-620. |
| 22 | 梁宗健. 单中心非透明细胞肾癌的临床病理特征和预后分析[D]. 重庆: 重庆医科大学, 2021. |
| 23 | 邓超, 宁刚.原发肾脏尤文肉瘤2例并文献复习[J].中国CT和MRI杂志,2022,20(6):180-182. |
| 24 | 毕海, 黄毅, 马潞林,等.3例肾尤文肉瘤合并下腔静脉癌栓的诊治[J].北京大学学报(医学版),2020,52(5):985-989. |
| 25 | 方三高.延胡索酸水合酶缺陷型肾细胞癌: 一种具有同类相食、淋巴细胞吞入和自噬缺陷等多种形态的肿瘤[J].诊断病理学杂志,2023,30(2):209. |
| 26 | XuY , KongW , CaoM ,et al.Genomic profiling and response to immune checkpoint inhibition plus tyrosine kinase inhibition in FH-deficient renal cell carcinoma[J].Eur Urol,2023,83(2):163-172. |
| 27 | 徐晓晨, 甘卫东, 李笑弓,等.Xp11.2易位/TFE3基因融合相关性肾癌与肾透明细胞癌的螺旋CT诊断鉴别[J].现代泌尿外科杂志,2012,17(2):122-124. |
| 28 | PintoK , ChettyR .Gene of the month: TFE3[J].J Clin Pathol,2020,73(11):691-694. |
| 29 | 刘德乾. Vimentin和Ki-67在肾癌中的表达及其临床意义[D]. 山东: 济宁医学院, 2018. |
| 30 | 谢星, 谭建明, 吴卫真.Ki-67和p53与肾癌的相关性研究[J].临床军医杂志,2011,39(3):445-446. |
| 31 | 戴津东, 张兴明, 曾浩.转移性肾癌减瘤性肾切除术的临床决策要点及挑战[J].临床外科杂志,2021,29(2):112-116. |
| 32 | 董毅, 王林辉.转移性肾癌减瘤性肾切除术的指征该如何把握[J].中华腔镜泌尿外科杂志(电子版),2019,13(5):289-292. |
| 33 | Patel HD, Karam JA, Allaf ME. Surgical management of advanced kidney cancer: The role of cytoreductive nephrectomy and lymphadenectomy [J]. J Clin Oncol, 2018, JCO2018790246. |
| 34 | 郭圣越, 王艳.抗血管生成联合免疫检查点抑制剂治疗晚期肾癌的理论基础及研究进展[J].现代肿瘤医学,2023,31(5):979-984. |
| 35 | 李浩, 张鹤骞, 高佳宁,等.立体定向体部放疗联合靶向药物治疗转移性肾癌的研究进展[J].实用肿瘤学杂志,2022,36(6):580-584. |
| [1] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [2] | 邱敏,宗有龙,王滨帅,杨斌,徐楚潇,孙争辉,陆敏,赵磊,卢剑,刘承,田晓军,马潞林. 腹腔镜肾部分切除术治疗中高复杂程度肾肿瘤的效果[J]. 北京大学学报(医学版), 2023, 55(5): 833-837. |
| [3] | 卢汉,张建运,杨榕,徐乐,李庆祥,郭玉兴,郭传瑸. 下颌牙龈鳞状细胞癌患者预后的影响因素[J]. 北京大学学报(医学版), 2023, 55(4): 702-707. |
| [4] | 时云飞,王豪杰,刘卫平,米岚,龙孟平,刘雁飞,赖玉梅,周立新,刁新婷,李向红. 血管免疫母细胞性T细胞淋巴瘤临床与分子病理学特征分析[J]. 北京大学学报(医学版), 2023, 55(3): 521-529. |
| [5] | 朱晓娟,张虹,张爽,李东,李鑫,徐玲,李挺. 人表皮生长因子受体2低表达乳腺癌的临床病理学特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 243-253. |
| [6] | 赖玉梅,李忠武,李欢,吴艳,时云飞,周立新,楼雨彤,崔传亮. 68例肛管直肠黏膜黑色素瘤临床病理特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 262-269. |
| [7] | 沈棋,刘亿骁,何群. 肾黏液样小管状和梭形细胞癌的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(2): 276-282. |
| [8] | 宿骞,彭歆,周传香,俞光岩. 369例口腔颌面部非霍奇金淋巴瘤的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(1): 13-21. |
| [9] | 张铨,宋海峰,马冰磊,张喆楠,周朝晖,李傲林,刘军,梁磊,朱时雨,张骞. 术前预后营养指数可作为预测非转移性肾细胞癌预后的指标[J]. 北京大学学报(医学版), 2023, 55(1): 149-155. |
| [10] | 邢晓燕,张筠肖,朱冯赟智,王一帆,周新尧,李玉慧. 皮肌炎合并巨噬细胞活化综合征5例[J]. 北京大学学报(医学版), 2022, 54(6): 1214-1218. |
| [11] | 曹乐清,周婧睿,陈育红,陈欢,韩伟,陈瑶,张圆圆,闫晨华,程翼飞,莫晓冬,付海霞,韩婷婷,吕萌,孔军,孙于谦,王昱,许兰平,张晓辉,黄晓军. 异基因造血干细胞移植后晚发重症肺炎患者治疗与预后转归的关系[J]. 北京大学学报(医学版), 2022, 54(5): 1013-1020. |
| [12] | 周利群,徐纯如. 机器人时代中央型肾肿瘤的手术治疗策略[J]. 北京大学学报(医学版), 2022, 54(4): 587-591. |
| [13] | 张崔建,何志嵩,周利群. 上尿路尿路上皮癌的淋巴清扫[J]. 北京大学学报(医学版), 2022, 54(4): 592-594. |
| [14] | 博尔术,洪鹏,张宇,邓绍晖,葛力源,陆敏,李楠,马潞林,张树栋. 乳头状肾细胞癌的临床病理特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(4): 615-620. |
| [15] | 邱敏,连岩岩,陆敏,王滨帅,田晓军,卢剑,刘承,张树栋,姜敏,马潞林. 多原发癌合并肾癌的治疗及预后[J]. 北京大学学报(医学版), 2022, 54(4): 680-685. |
|
||