北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (5): 793-801. doi: 10.19723/j.issn.1671-167X.2023.05.004
基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估
- 1. 重庆医科大学附属第一医院泌尿外科, 重庆 400016
2. 分子肿瘤与表观遗传学重庆市重点实验室, 重庆 400016
Risk modeling based on HER-2 related genes for bladder cancer survival prognosis assessment
Huan-rui LIU1,Xiang PENG1,2,Sen-lin LI1,Xin GOU1,*( )
)
- 1. Department of Urology, The First Hospital of Chongqing Medical University, Chongqing 400016, China
2. Chongqing Key Laboratory of Molecular Tumor and Epigenetics, Chongqing 400016, China
摘要:
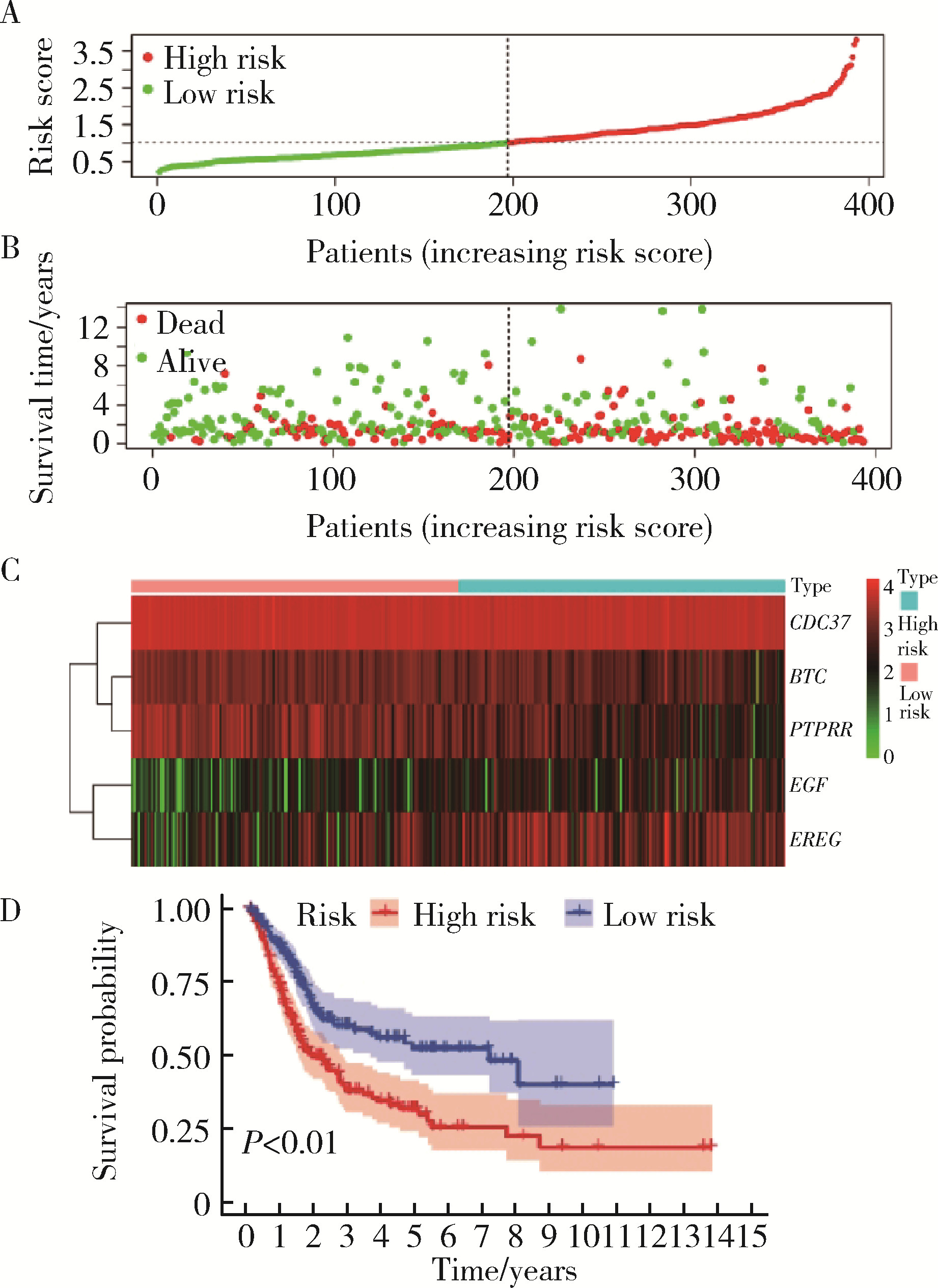
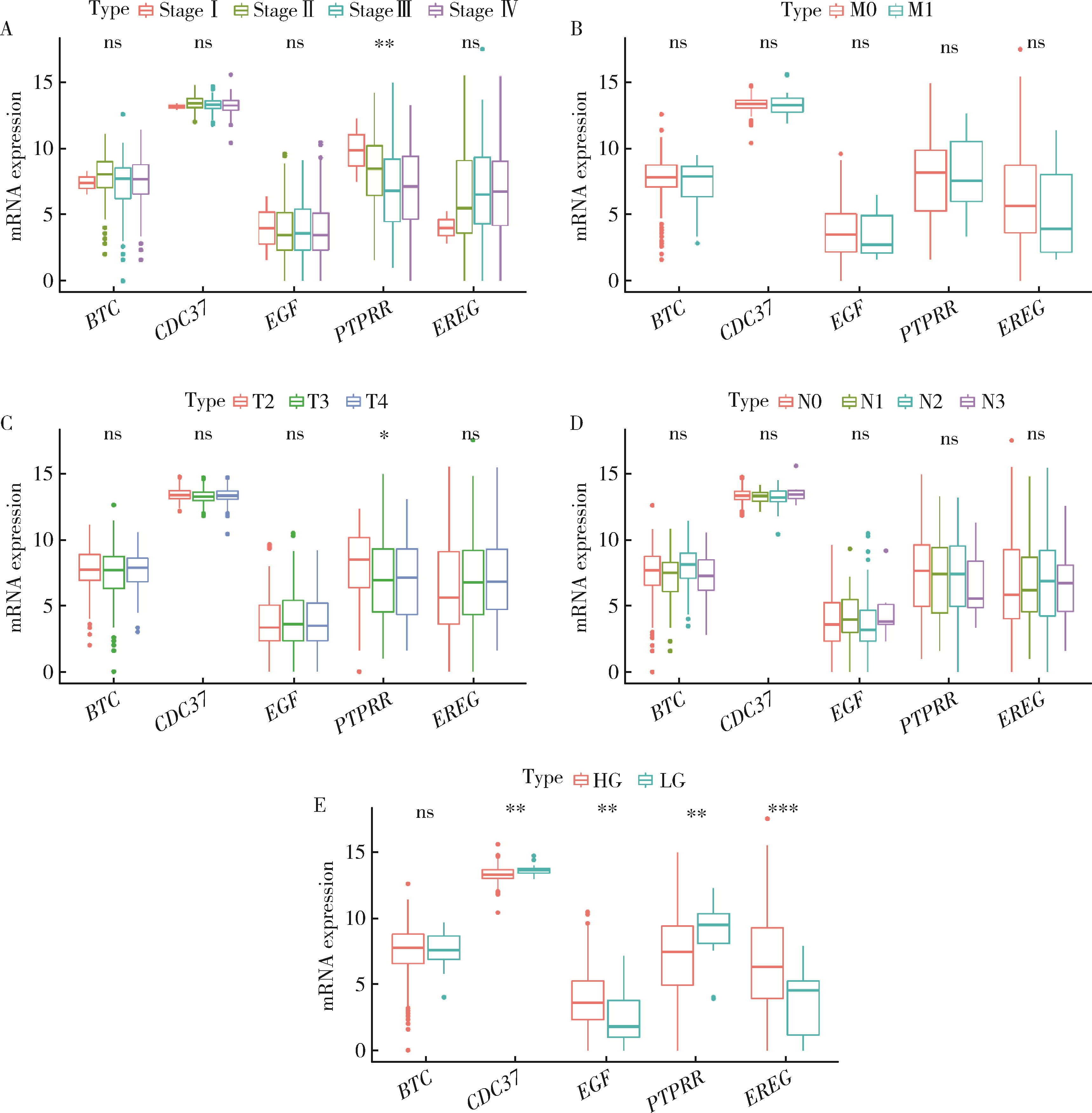
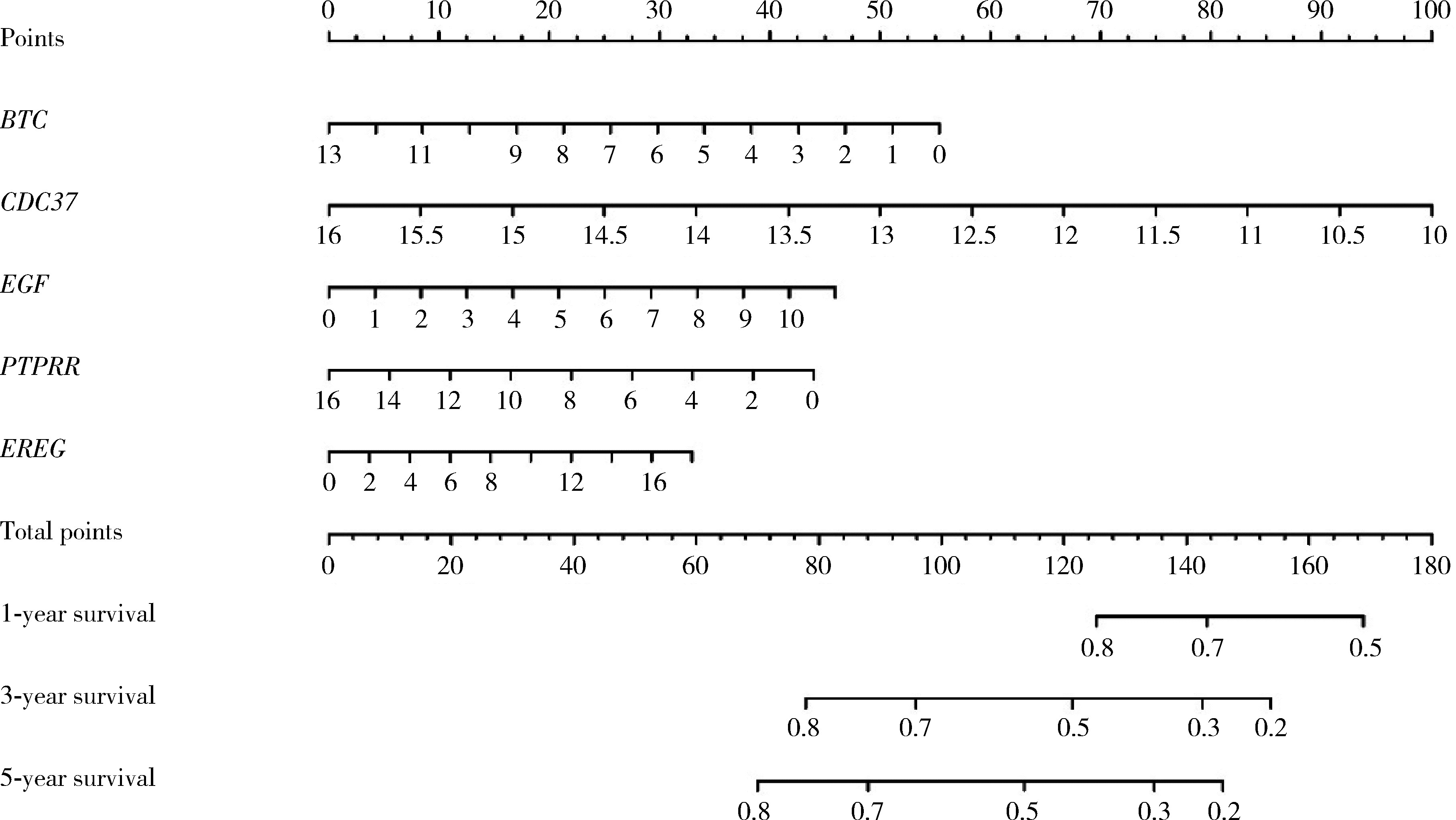
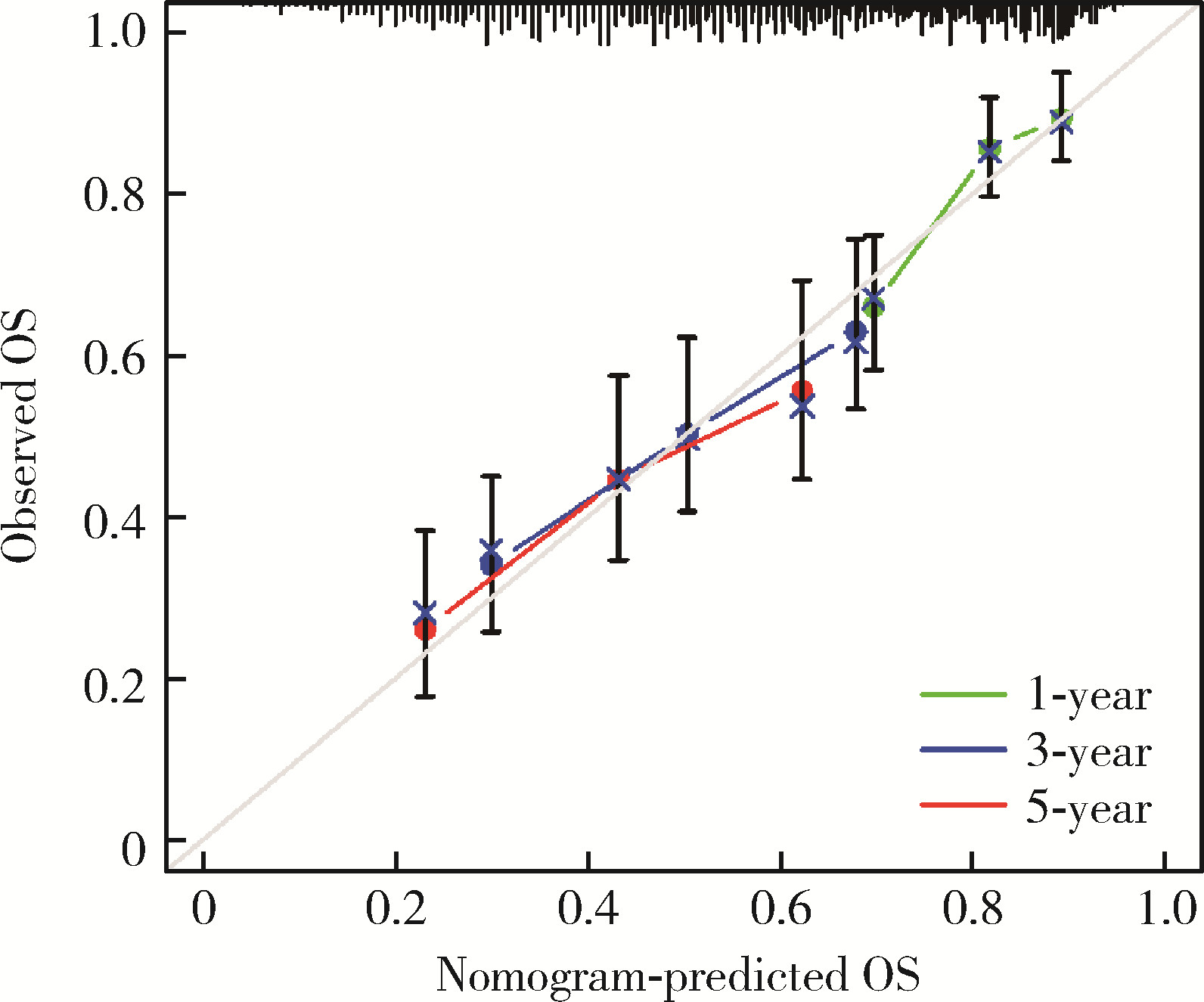
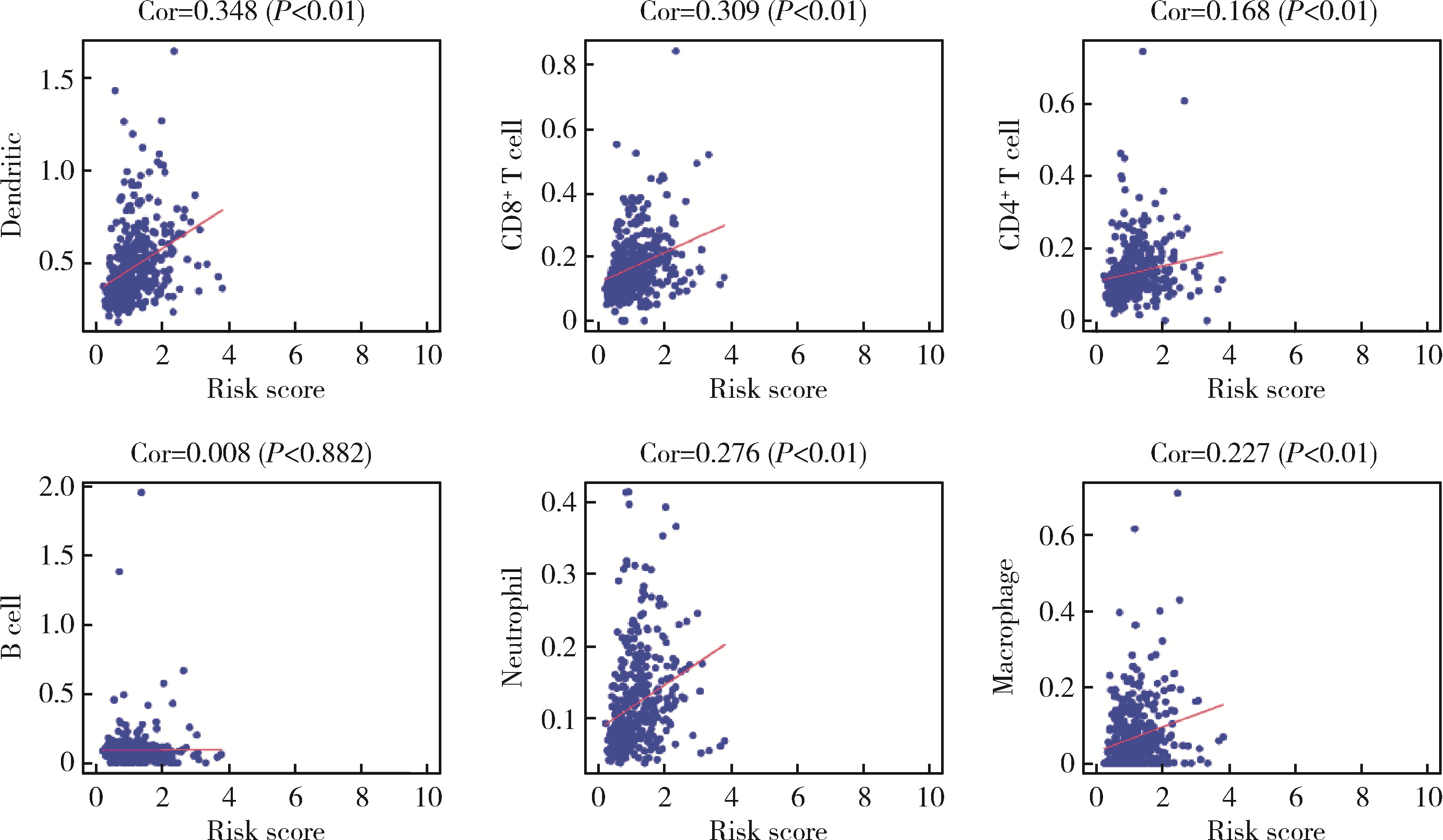
目的: 探讨HER-2相关基因(the human epidermal growth factor receptor-2-related genes, HRGs)与膀胱癌生存预后的相关性,并基于HRGs构建一种膀胱癌患者生存预后的预测模型。方法: 从癌症基因组图谱(the cancer genome atlas, TCGA)中下载膀胱肿瘤组织mRNA测序数据和临床数据,通过与分子签名数据库(the molecular signatures database, MSigDB)中HER-2相关的基因联合分析鉴定膀胱癌中的HRGs。利用单因素和多因素Cox回归分析进一步明确与膀胱癌生存相关的HRGs(P < 0.05),并构建HRGs风险模型(HRGs risk score model, HRSM),根据风险评分取中位数将膀胱癌患者分成高风险组和低风险组。利用R语言对高风险和低风险组的患者进行生存分析,并对HRGs与临床特征的相关性进行分析。利用多因素Cox回归分析,验证影响膀胱癌患者预后的独立因素。计算HRSM的受试者工作特征曲线(receiver operating characteristic curve, ROC)下的面积(area under the curve, AUC),并构建诺模图(nomogram)对膀胱癌患者进行生存预测。利用TIMER数据库对HRSM和患者免疫细胞浸润相关性进行分析。结果: 共鉴定到13个与患者生存相关的HRGs。通过多因素Cox回归分析,筛选出5个基因(BTC、CDC37、EGF、PTPRR和EREG)构建HRSM,高风险组的膀胱癌患者5年生存率明显低于低风险组患者。通过临床相关性分析发现,PTPRR的高表达与肿瘤分级、分期呈显著负相关,而EREG的高表达与肿瘤分级、分期呈正相关;EGF表达量的增加和患者的高级别有相关性,而CDC37的高表达却呈现出了相反的结果;BTC的表达与临床特征无显著相关性。通过对HRSM与免疫细胞的相关性分析发现,风险评分与树突状细胞、CD8+T细胞、CD4+T细胞、中性粒细胞和巨噬细胞的浸润呈正相关。结论: HRGs对膀胱癌患者的预后有重要作用,可能作为新的预测性生物标志物和治疗的潜在靶点。
中图分类号:
- R737.1
| 1 |
AneoniS , FerlayJ , SoerjomatarmI ,et al.Bladder cancer incidence and mortality: A global overview and recent trends[J].Eur Urol,2017,71(1):96-108.
doi: 10.1016/j.eururo.2016.06.010 |
| 2 |
NielsenME , SmithAB , MererAM ,et al.Trends in stage-specific incidence rates for urothelial carcinoma of the bladder in the Uni-ted States: 1988 to 2006[J].Cancer,2014,120(1):86-95.
doi: 10.1002/cncr.28397 |
| 3 |
CrispenPL , KusmartsevS .Mechanisms of immune evasion in bladder cancer[J].Cancer Immunol Immunother,2020,69(1):3-14.
doi: 10.1007/s00262-019-02443-4 |
| 4 |
Goossens-LaanCA , LeliveldAM , VerhoevenRH ,et al.Effects of age and comorbidity on treatment and survival of patients with muscle-invasive bladder cancer[J].Int J Cancer,2014,135(4):905-912.
doi: 10.1002/ijc.28716 |
| 5 | Redondo-GonzalezE , de CastroLN , Moreno-SierraJ ,et al.Bladder carcinoma data with clinical risk factors and molecular mar-kers: A cluster analysis[J].Biomed Res Int,2015,2015,168682. |
| 6 |
MoasserMM .The oncogene HER2 : Its signaling and transforming functions and its role in human cancer pathogenesis[J].Oncogene,2007,26(45):6469-6487.
doi: 10.1038/sj.onc.1210477 |
| 7 |
BegnamiMD , FukudaE , FregnaniJH ,et al.Prognostic implications of altered human epidermal growth factor receptors (HERs) in gastric carcinomas: HER2 and HER3 are predictors of poor outcome[J].J Clin Oncol,2011,29(22):3030-3036.
doi: 10.1200/JCO.2010.33.6313 |
| 8 |
BangYJ , van CutsemE , FeyereislovaA ,et al.Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial[J].Lancet,2010,376(9742):687-697.
doi: 10.1016/S0140-6736(10)61121-X |
| 9 |
WolffAC , HammondME , HicksDG ,et al.Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Patho-logists clinical practice guideline update[J].J Clin Oncol,2013,31(31):3997-4013.
doi: 10.1200/JCO.2013.50.9984 |
| 10 |
IyerG , Al-AhmadieH , SchultzN ,et al.Prevalence and co-occurrence of actionable genomic alterations in high-grade bladder cancer[J].J Clin Oncol,2013,31(25):3133-3140.
doi: 10.1200/JCO.2012.46.5740 |
| 11 |
BaiX , HeW , YinH ,et al.Prognostic significance of HER2 status evaluation using immunohistochemistry in patients with urothelial carcinoma of the bladder: A retrospective single-center experience[J].Exp Ther Med,2022,24(5):704.
doi: 10.3892/etm.2022.11640 |
| 12 |
LoiS , SirtaineN , PietteF ,et al.Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase Ⅲ randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98[J].J Clin Oncol,2013,31(7):860-867.
doi: 10.1200/JCO.2011.41.0902 |
| 13 |
StantonSE , AdamsS , DisisML .Variation in the incidence and magnitude of tumor-infiltrating lymphocytes in breast cancer subtypes: A systematic review[J].JAMA Oncol,2016,2(10):1354-1360.
doi: 10.1001/jamaoncol.2016.1061 |
| 14 |
JiaY , KodumudiKN , RamamoorthiG ,et al.Th1 cytokine interferon gamma improves response in HER2 breast cancer by modulating the ubiquitin proteasomal pathway[J].Mol Ther,2021,29(4):1541-1556.
doi: 10.1016/j.ymthe.2020.12.037 |
| 15 |
WülfingC , MachielsJP , RichelDJ ,et al.A single-arm, multicenter, open-label phase 2 study of lapatinib as the second-line treatment of patients with locally advanced or metastatic transitional cell carcinoma[J].Cancer,2009,115(13):2881-2890.
doi: 10.1002/cncr.24337 |
| 16 |
ShengX , YanX , WangL ,et al.Open-label, multicenter, phase Ⅱ study of RC48-ADC, a HER2-targeting antibody-drug conjugate, in patients with locally advanced or metastatic urothelial carcinoma[J].Clin Cancer Res,2021,27(1):43-51.
doi: 10.1158/1078-0432.CCR-20-2488 |
| 17 | ShengX , ZhouAP , YaoX ,et al.A phase Ⅱ study of RC48-ADC in HER2-positive patients with locally advanced or metastatic urothelial carcinoma[J].J Clin Oncol,2019,37(Suppl 15):4509. |
| 18 |
RushJS , PetersonJL , CeresaBP .Betacellulin (BTC) biases the EGFR to dimerize with ErbB3[J].Mol Pharmacol,2018,94(6):1382-1390.
doi: 10.1124/mol.118.113399 |
| 19 |
ShenT , YangT , YaoM ,et al.BTC as a novel biomarker contri-buting to EMT via the PI3K-AKT pathway in OSCC[J].Front Genet,2022,13,875617.
doi: 10.3389/fgene.2022.875617 |
| 20 |
DahlhoffM , WolfE , SchneiderMR .The ABC of BTC: Structural properties and biological roles of betacellulin[J].Semin Cell Dev Biol,2014,28,42-48.
doi: 10.1016/j.semcdb.2014.01.002 |
| 21 |
OlsenDA , KjaerIM , BrandslundI .Development of a three-plex single molecule immunoassay enabling measurement of the EGFR ligands amphiregulin, betacellulin and transforming growth factor alpha simultaneously in human serum samples[J].J Immunol Methods,2018,459,63-69.
doi: 10.1016/j.jim.2018.05.002 |
| 22 | LeeYS , SongGJ , JunHS .Betacellulin-induced alpha-cell proli-feration is mediated by ErbB3 and ErbB4, and may contribute to beta-cell regeneration[J].Front Cell Dev Biol,2020,8,605110. |
| 23 | OlsenDA , BechmannT , ϕstergaardB ,et al.Increased concentrations of growth factors and activation of the EGFR system in breast cancer[J].Clin Chem Lab Med,2012,50(10):1809-1818. |
| 24 |
PearlLH .Hsp90 and Cdc37: A chaperone cancer conspiracy[J].Curr Opin Genet Dev,2005,15(1):55-61.
doi: 10.1016/j.gde.2004.12.011 |
| 25 |
SerwetnykMA , BlaggBSJ .The disruption of protein-protein interactions with co-chaperones and client substrates as a strategy towards Hsp90 inhibition[J].Acta Pharm Sin B,2021,11(6):1446-1468.
doi: 10.1016/j.apsb.2020.11.015 |
| 26 |
GrayPJ , Jr. , PrinceT , ChengJ ,et al.Targeting the oncogene and kinome chaperone CDC37[J].Nat Rev Cancer,2008,8(7):491-495.
doi: 10.1038/nrc2420 |
| 27 |
GhatakS , MisraS , TooleBP .Hyaluronan constitutively regulates ErbB2 phosphorylation and signaling complex formation in carcinoma cells[J].J Biol Chem,2005,280(10):8875-8883.
doi: 10.1074/jbc.M410882200 |
| 28 |
HuangW , YeM , ZhangLR ,et al.FW-04-806 inhibits proliferation and induces apoptosis in human breast cancer cells by binding to N-terminus of Hsp90 and disrupting Hsp90-Cdc37 complex formation[J].Mol Cancer,2014,13,150.
doi: 10.1186/1476-4598-13-150 |
| 29 |
Esparís-OgandoA , MonteroJC , ArribasJ ,et al.Targeting the EGF/HER ligand-receptor system in cancer[J].Curr Pharm Des,2016,22(39):5887-5898.
doi: 10.2174/1381612822666160715132233 |
| 30 | WangZ .ErbB receptors and cancer[J].Methods Mol Biol,2017,1652,3-35. |
| 31 | GarousiS , Jahanbakhsh-GodehkahrizS , EsfahaniK ,et al.Meta-analysis of EGF-stimulated normal and cancer cell lines to discover EGF-associated oncogenic signaling pathways and prognostic biomarkers[J].Iran J Biotechnol,2022,20(3):e3245. |
| 32 | LaczmanskaI , SasiadekMM .Tyrosine phosphatases as a superfamily of tumor suppressors in colorectal cancer[J].Acta Biochim Pol,2011,58(4):467-470. |
| 33 |
MenigattiM , CattaneoE , Sabates-BellverJ ,et al.The protein tyrosine phosphatase receptor type R gene is an early and frequent target of silencing in human colorectal tumorigenesis[J].Mol Cancer,2009,8,124.
doi: 10.1186/1476-4598-8-124 |
| 34 |
WangY , CaoJ , LiuW ,et al.Protein tyrosine phosphatase receptor type R (PTPRR) antagonizes the wnt signaling pathway in ovarian cancer by dephosphorylating and inactivating β-catenin[J].J Biol Chem,2019,294(48):18306-18323.
doi: 10.1074/jbc.RA119.010348 |
| 35 |
SuPH , LinYW , HuangRL ,et al.Epigenetic silencing of PTPRR activates MAPK signaling, promotes metastasis and serves as a biomarker of invasive cervical cancer[J].Oncogene,2013,32(1):15-26.
doi: 10.1038/onc.2012.29 |
| 36 |
MunkleyJ , LaffertyNP , KalnaG ,et al.Androgen-regulation of the protein tyrosine phosphatase PTPRR activates ERK1/2 signalling in prostate cancer cells[J].BMC Cancer,2015,15,9.
doi: 10.1186/s12885-015-1012-8 |
| 37 |
ChengWL , FengPH , LeeKY ,et al.The role of EREG/EGFR pathway in tumor progression[J].Int J Mol Sci,2021,22(23):12828.
doi: 10.3390/ijms222312828 |
| 38 |
ZhangL , NanF , YangL ,et al.Differentially expressed EREG and SPP1 are independent prognostic markers in cervical squamous cell carcinoma[J].J Obstet Gynaecol Res,2022,48(7):1848-1858.
doi: 10.1111/jog.15265 |
| 39 |
LiuS , WangY , HanY ,et al.EREG-driven oncogenesis of head and neck squamous cell carcinoma exhibits higher sensitivity to erlotinib therapy[J].Theranostics,2020,10(23):10589-10605.
doi: 10.7150/thno.47176 |
| 40 |
XiaQ , ZhouY , YongH ,et al.Elevated epiregulin expression predicts poor prognosis in gastric cancer[J].Pathol Res Pract,2019,215(5):873-879.
doi: 10.1016/j.prp.2019.01.030 |
| [1] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [2] | 刘帅,刘磊,刘茁,张帆,马潞林,田晓军,侯小飞,王国良,赵磊,张树栋. 伴静脉癌栓的肾上腺皮质癌的临床治疗及预后[J]. 北京大学学报(医学版), 2024, 56(4): 624-630. |
| [3] | 虞乐,邓绍晖,张帆,颜野,叶剑飞,张树栋. 具有低度恶性潜能的多房囊性肾肿瘤的临床病理特征及预后[J]. 北京大学学报(医学版), 2024, 56(4): 661-666. |
| [4] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [5] | 方杨毅,李强,黄志高,陆敏,洪锴,张树栋. 睾丸鞘膜高分化乳头状间皮肿瘤1例[J]. 北京大学学报(医学版), 2024, 56(4): 741-744. |
| [6] | 刘佐相,陈晓薇,赵厚宇,詹思延,孙凤. 真实世界中2型糖尿病患者二甲双胍联用西格列汀的心血管安全性[J]. 北京大学学报(医学版), 2024, 56(3): 424-430. |
| [7] | 曾媛媛,谢云,陈道南,王瑞兰. 脓毒症患者发生正常甲状腺性病态综合征的相关因素[J]. 北京大学学报(医学版), 2024, 56(3): 526-532. |
| [8] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [9] | 李建斌,吕梦娜,池强,彭一琳,刘鹏程,吴锐. 干燥综合征患者发生重症新型冠状病毒肺炎的早期预测[J]. 北京大学学报(医学版), 2023, 55(6): 1007-1012. |
| [10] | 薛子璇,唐世英,邱敏,刘承,田晓军,陆敏,董靖晗,马潞林,张树栋. 青年肾肿瘤伴瘤栓的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2023, 55(5): 802-811. |
| [11] | 卢汉,张建运,杨榕,徐乐,李庆祥,郭玉兴,郭传瑸. 下颌牙龈鳞状细胞癌患者预后的影响因素[J]. 北京大学学报(医学版), 2023, 55(4): 702-707. |
| [12] | 时云飞,王豪杰,刘卫平,米岚,龙孟平,刘雁飞,赖玉梅,周立新,刁新婷,李向红. 血管免疫母细胞性T细胞淋巴瘤临床与分子病理学特征分析[J]. 北京大学学报(医学版), 2023, 55(3): 521-529. |
| [13] | 朱晓娟,张虹,张爽,李东,李鑫,徐玲,李挺. 人表皮生长因子受体2低表达乳腺癌的临床病理学特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 243-253. |
| [14] | 赖玉梅,李忠武,李欢,吴艳,时云飞,周立新,楼雨彤,崔传亮. 68例肛管直肠黏膜黑色素瘤临床病理特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 262-269. |
| [15] | 沈棋,刘亿骁,何群. 肾黏液样小管状和梭形细胞癌的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(2): 276-282. |
|
||