北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (6): 1119-1123. doi: 10.19723/j.issn.1671-167X.2019.06.025
后牙种植冠桥修复后局部咬合变化的定量分析
- 1. 中国人民解放军总医院口腔医学中心,北京 100853
2. 北京大学口腔医学院·口腔医院,修复科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100081
Quantitative analysis of occlusal changes in posterior partial fixed implant supported prostheses
Qiang LUO1,Qian DING2,Lei ZHANG2,△( ),Qiu-fei XIE2
),Qiu-fei XIE2
- 1. Institute of Stomatology, General Hospital of Chinese PLA, Beijing 100853, China
2. Department of Prosthodontics, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
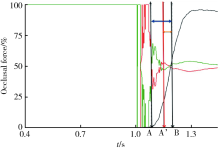
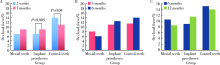
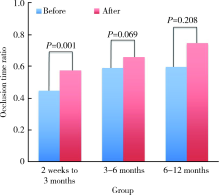
目的 定量分析后牙种植冠桥修复后局部咬合力与咬合接触的变化规律,为种植修复体的精确咬合设计、调整和维护提供参考。方法 按照一定的纳入和排除标准收集后牙区缺牙并行种植单冠或固定桥修复的患者,分别于修复后2周、3个月、6个月、12个月复查,采用咬合纸和T-Scan Ⅲ ?(Tekscan,South Boston,USA)电子咬合分析系统检查全牙列咬合接触情况,分别记录每个时间点对照牙、近中邻牙和种植修复体的咬合接触时间和咬合力百分比,分析局部咬合接触和咬合力随时间的变化。结果 共收集33例患者(男性16人,女性17人,年龄24~72岁)、37颗种植修复体,修复体戴用3~12个月(平均8.3个月)。2周到3个月,种植修复体达到咬合接触的时间显著缩短(P<0.05,Wilcoxon检验),种植修复体的咬合力百分比显著增大(P<0.05,Wilcoxon检验);3~6个月、6~12个月期间,咬合力百分比和咬合接触时间变化均不明显。2周时,种植修复体咬合力显著低于对照牙(P<0.01),而戴用3个月后种植修复体咬合力与对照牙差异已无统计学意义,6个月、12个月时差异均无统计学意义。结论 轻咬合接触和咬合接触时间延迟的后牙种植修复体,在修复后3个月咬合接触强度会明显增加,临床上种植修复后3个月复查时应重点关注咬合情况。
中图分类号:
- R783.3
| [1] | Zembic A, Kim S, Zwahlen M , et al. Systematic review of the survival rate and incidence of biologic, technical, and esthetic complications of single implant abutments supporting fixed prostheses[J]. Int J Oral Maxillofac Implants, 2014,29(Suppl):99-116. |
| [2] | Velzen FJ, Ofec R, Schulten EA , et al. 10-year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients[J]. Clin Oral Implants Res, 2015,26(10):1121-1128. |
| [3] | Jung RE, Zembic A, Pjetursson BE , et al. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years[J]. Clin Oral Implants Res, 2012,23(Suppl 6):2-21. |
| [4] | Lee JH, Lee JB, Park JI , et al. Mechanical complication rates and optimal horizontal distance of the most distally positioned implant-supported single crowns in the posterior region: a study with a mean follow-up of 3 years[J]. J Prosthodont, 2015,24(7):517-524. |
| [5] | Anner R, Grossmann Y, Anner Y , et al. Smoking, diabetes mellitus, periodontitis, and supportive periodontal treatment as factors associated with dental implant survival: a long-term retrospective evaluation of patients followed for up to 10 years[J]. Implant Dent, 2010,19(1):57-64. |
| [6] | Kim Y, Oh TJ, Misch CE , et al. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale[J]. Clin Oral Implants Res, 2005,16(1):26-35. |
| [7] | Goodacre CJ, Bernal G, Rungcharassaeng K , et al. Clinical complications with implants and implant prostheses[J]. J Prosthet Dent, 2003,90(2):121-132. |
| [8] | Yuan JC, Sukotjo C . Occlusion for implant-supported fixed dental prostheses in partially edentulous patients: a literature review and current concepts[J]. J Periodontal Implant Sci, 2013,43(2):51-57. |
| [9] | Bocklage R . Biomechanical aspects of monoblock implant bridges for the edentulous maxilla and mandible: concepts of occlusion and articulation[J]. Implant Dent, 2004,13(1):49-53. |
| [10] | Kerstein RB . Nonsimultaneous tooth contact in combined implant and natural tooth occlusal schemes[J]. Pract Proced Aesthet Dent, 2001,13(9):751-755. |
| [11] | Stevens CJ . Computerized occlusal implant management with the T-Scan II System: a case report[J]. Dent Today, 2006,25(2):88-91. |
| [12] | Lewis MB, Klineberg I . Prosthodontic considerations designed to optimize outcomes for single-tooth implants. A review of the literature[J]. Aust Dent J, 2011,56(2):181-192. |
| [13] | Roberts SD, Kapadia H, Greenlee G , et al. Midfacial and dental changes associated with nasal positive airway pressure in children with obstructive sleep apnea and craniofacial conditions[J]. J Clin Sleep Med, 2016,12(4):469-475. |
| [14] | D’Incau E, Couture C, Maureille B . Human tooth wear in the past and the present: tribological mechanisms, scoring systems, dental and skeletal compensations[J]. Arch Oral Biol, 2012,57(3):214-229. |
| [15] | Mundhe K, Jain V, Pruthi G , et al. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns[J]. J Prosthet Dent, 2015,114(3):358-365. |
| [16] | Palaniappan S, Elsen L, Lijnen I , et al. Nanohybrid and microfilled hybrid versus conventional hybrid composite restorations: 5-year clinical wear performance[J]. Clinl Oral Investig, 2012,16(1):181-190. |
| [17] | Heij DG, Opdebeeck H, van Steenberghe D, et al. Facial deve-lopment, continuous tooth eruption, and mesial drift as compromising factors for implant placement[J]. Int J Oral Maxillofac Implants, 2006,21(6):867-878. |
| [18] | Schulte W . Implants and the periodontium[J]. Int Dent J, 1995,45(1):16-26. |
| [19] | Kerstein RB, Radke J . Clinician accuracy when subjectively interpreting articulating paper markings[J]. Cranio, 2014,32(1):13-23. |
| [20] | Koos B, Godt A, Schille C , et al. Precision of an instrumentation-based method of analyzing occlusion and its resulting distribution of forces in the dental arch[J]. J Orofac Orthop, 2010,71(6):403-410. |
| [1] | 王聪伟,高敏,于尧,章文博,彭歆. 游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析[J]. 北京大学学报(医学版), 2024, 56(1): 66-73. |
| [2] | 李穗,马雯洁,王时敏,丁茜,孙瑶,张磊. 上前牙种植单冠修复体切导的数字化设计正确度[J]. 北京大学学报(医学版), 2024, 56(1): 81-87. |
| [3] | 刘晓强,周寅. 牙种植同期植骨术围术期高血压的相关危险因素[J]. 北京大学学报(医学版), 2024, 56(1): 93-98. |
| [4] | 丁茜,李文锦,孙丰博,谷景华,林元华,张磊. 表面处理对氧化钇和氧化镁稳定的氧化锆种植体晶相及断裂强度的影响[J]. 北京大学学报(医学版), 2023, 55(4): 721-728. |
| [5] | 欧蒙恩,丁云,唐卫峰,周永胜. 基台边缘-牙冠的平台转移结构中粘接剂流动的三维有限元分析[J]. 北京大学学报(医学版), 2023, 55(3): 548-552. |
| [6] | 孙菲,刘建,李思琪,危伊萍,胡文杰,王翠. 种植体黏膜下微生物在健康种植体和种植体周炎中的构成与差异:一项横断面研究[J]. 北京大学学报(医学版), 2023, 55(1): 30-37. |
| [7] | 王鹃,尉华杰,孙井德,邱立新. 预成刚性连接杆用于无牙颌种植即刻印模制取的应用评价[J]. 北京大学学报(医学版), 2022, 54(1): 187-192. |
| [8] | 梁峰,吴敏节,邹立东. 后牙区单牙种植修复5年后的临床修复疗效观察[J]. 北京大学学报(医学版), 2021, 53(5): 970-976. |
| [9] | 刘晓强,杨洋,周建锋,刘建彰,谭建国. 640例单牙种植术对血压和心率影响的队列研究[J]. 北京大学学报(医学版), 2021, 53(2): 390-395. |
| [10] | 周培茹, 蒋析, 华红. 口腔黏膜病患者口腔种植的时机及注意事项[J]. 北京大学学报(医学版), 2021, 53(1): 5-8. |
| [11] | 李蓬,朴牧子,胡洪成,王勇,赵一姣,申晓婧. 经嵴顶上颌窦底提升术后不植骨同期种植的影像研究[J]. 北京大学学报(医学版), 2021, 53(1): 95-101. |
| [12] | 郝柯屹,罗佳,邸萍,郭厚佐,沈惠丹,刘焱萍,张宇,林野. 三维图像融合技术评价上颌全牙列种植固定修复前后的鼻唇软组织形态变化[J]. 北京大学学报(医学版), 2020, 52(5): 924-930. |
| [13] | 李维婷,李蓬,朴牧子,张芳,邸杰. 不同备洞方法收集自体骨骨量[J]. 北京大学学报(医学版), 2020, 52(1): 103-106. |
| [14] | 李琳琳,赵一姣,陈虎,王勇,孙玉春. 转移牙合架固定法三维重建牙尖交错牙合的精度评价[J]. 北京大学学报(医学版), 2020, 52(1): 138-143. |
| [15] | 萧宁,孙玉春,赵一姣,王勇. 三种数字化分析算法测量咬合接触分布及面积的对比研究[J]. 北京大学学报(医学版), 2020, 52(1): 144-151. |
|
||