北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (3): 470-478. doi: 10.19723/j.issn.1671-167X.2020.03.012
孕早期血清维生素E水平与妊娠期高血压疾病发病风险的关系
孟文颖1,黄琬桐2,张杰2,焦明远3,金蕾4,靳蕾2,△( )
)
- 1. 北京市通州区妇幼保健院产科,北京 101100
2. 北京大学生育健康研究所,国家卫生健康委员会生育健康重点实验室,北京大学公共卫生学院流行病与卫生统计学系,北京 100191
3. 北京市通州区妇幼保健院检验科,北京 101100
4. 北京市通州区妇幼保健院妇女保健科,北京 101100
Relationship between serum vitamin E concentration in first trimester and the risk of developing hypertension disorders complicating pregnancy
Wen-ying MENG1,Wan-tong HUANG2,Jie ZHANG2,Ming-yuan JIAO3,Lei JIN4,Lei JIN2,△( )
)
- 1. Department of Obstetrics, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
2. Institute of Reproductive and Child Health, National Health Commission Key Laboratory of Reproductive Health, Peking University, Beijing 100191, China; Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
3. Department of Clinical Laboratory, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
4. Department of Maternal Health Care, Tongzhou Maternal & Child Health Hospital of Beijing, Beijing 101100, China
摘要:
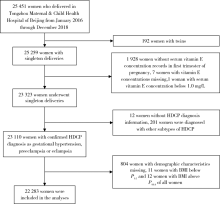
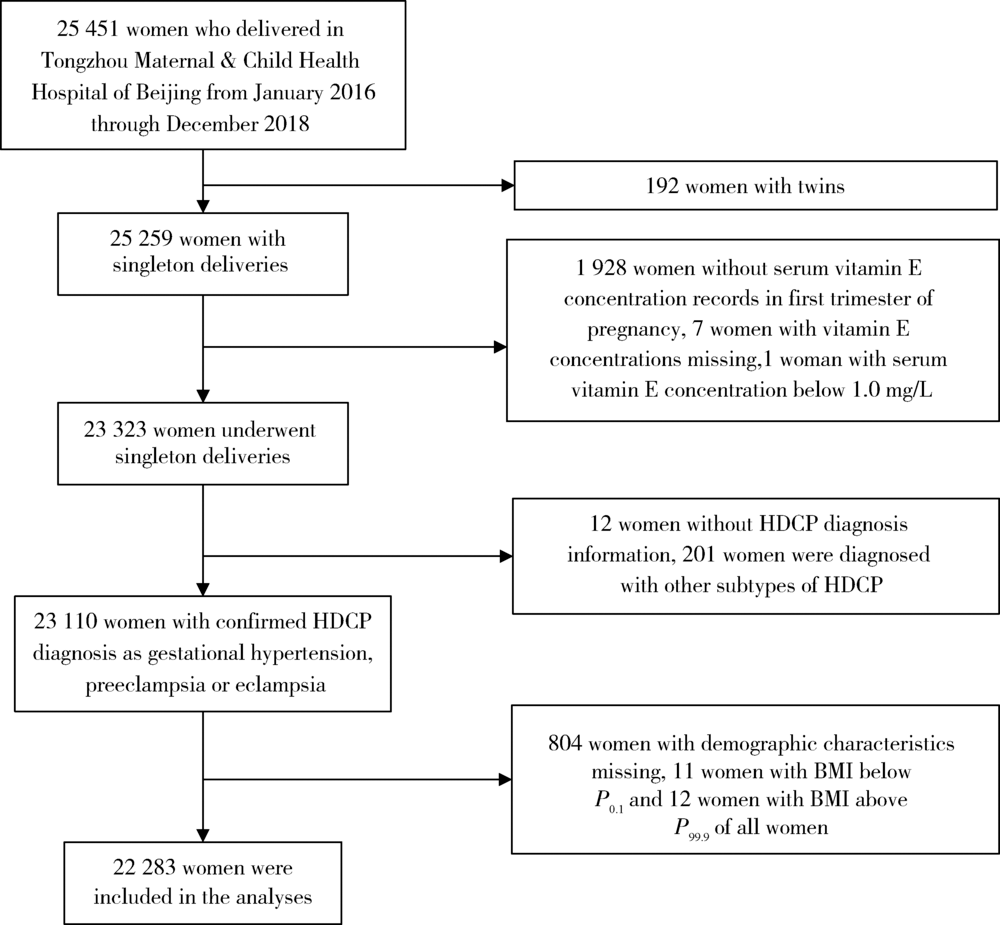
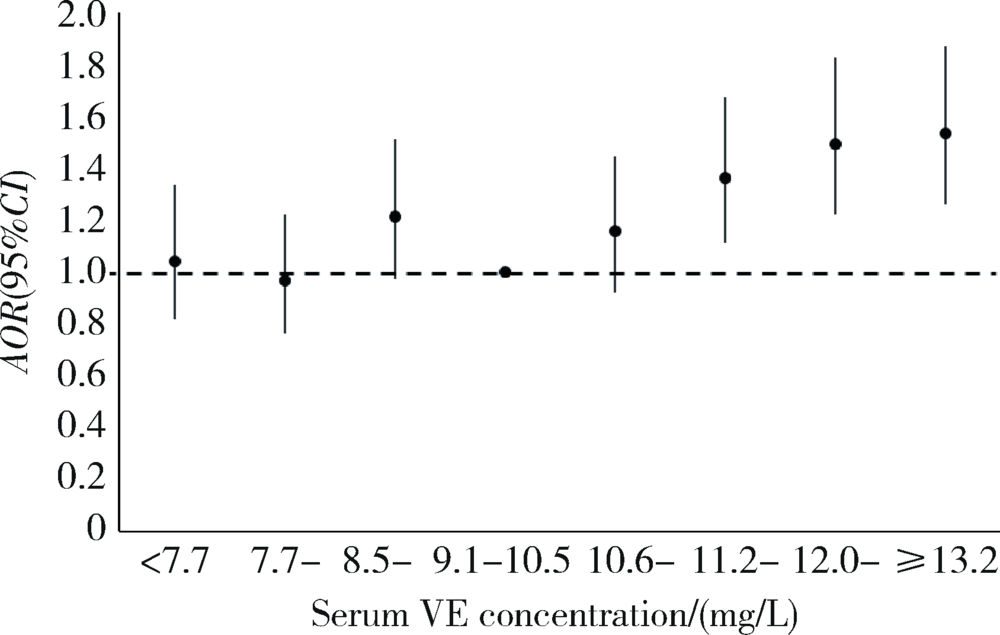
目的 了解北京妇女妊娠期高血压疾病(hypertension disorders complicating pregnancy, HDCP)发病率和孕早期维生素E(vitamin E, VE)营养状况,探究孕早期血清VE浓度与HDCP发病率的关系。方法 以北京市通州区孕期保健系统和通州区妇幼保健院医院信息系统为基础,利用2016年1月至 2018年12月在北京市通州区妇幼保健院分娩并在孕早期测定了血清VE浓度的22 283名单胎孕产妇的信息进行回顾性队列研究,用非条件Logistic回归模型分析不同血清VE浓度与HDCP发病风险的关系。结果 HDCP总发病率为5.4%,其中妊娠期高血压发病率为2.1%,子痫前期-子痫发病率为3.3%。妇女孕早期血清VE浓度中位值为10.1(8.8 ~ 11.6) mg/L,99.7%的妇女孕早期血清VE水平处于正常参考值范围内。3年间,妇女孕早期血清VE浓度(P < 0.001)及HDCP的发病率(P = 0.005)均有逐年上升趋势。单因素与多因素Logistic回归分析结果显示,血清VE浓度较高的孕妇HDCP的发病风险更高;在多因素Logistic回归分析中,与血清VE浓度在百分位数
中图分类号:
- R172
| [1] | 谢幸, 苟文丽. 妇产科学[M]. 8版. 北京: 人民卫生出版社, 2013: 42, 64. |
| [2] | 中华医学会妇产科学分会妊娠期高血压疾病学组. 妊娠期高血压疾病诊治指南(2015)[J]. 中华围产医学杂志, 2016,19(3):161-169. |
| [3] |
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis[J]. Hypertens Res, 2017,40(3):213-220.
pmid: 27682655 |
| [4] | Ye C, Ruan Y, Zou L, et al. The 2011 survey on hypertensive disorders of pregnancy (HDP) in China: prevalence, risk factors, complications, pregnancy and perinatal outcomes[J]. PLoS One, 2014,9(6):e100180. |
| [5] |
You SH, Cheng PJ, Chung TT, et al. Population-based trends and risk factors of early- and late-onset preeclampsia in Taiwan 2001—2014[J]. BMC Pregnancy Childbirth, 2018,18(1):199.
pmid: 29855344 |
| [6] | Paré E, Parry S, McElrath TF, et al. Clinical risk factors for preeclampsia in the 21st century[J]. Obstet Gynecol, 2014,124(4):763-770. |
| [7] |
Redman CW, Sargent IL. Latest advances in understanding preeclampsia[J]. Science, 2005,308(5728):1592-1594.
pmid: 15947178 |
| [8] | 殷为, 钟梅. 妊娠期高血压疾病的病因、预测及诊疗进展[J]. 实用医学杂志, 2016,32(11):1887-1890. |
| [9] | 孙长颢. 营养与食品卫生学[M]. 8版. 北京: 人民卫生出版社, 2017: 93-95, 215. |
| [10] | 郭方, 李笑天. 叶酸及多种维生素的补充对妊娠期高血压疾病的预防作用[J]. 中国实用妇科与产科杂志, 2014,30(8):592-596. |
| [11] | Rumbold A, Ota E, Hori H, et al. Vitamin E supplementation in pregnancy[J]. Cochrane Database Syst Rev, 2015(9): CD004069. |
| [12] |
Zhang C, Williams MA, Sanchez SE, et al. Plasma concentrations of carotenoids, retinol, and tocopherols in preeclamptic and normotensive pregnant women[J]. Am J Epidemiol, 2001,153(6):572-580.
pmid: 11257065 |
| [13] | Roberts JM, Myatt L, Spong CY, et al. Vitamins C and E to prevent complications of pregnancy-associated hypertension[J]. N Engl J Med, 2010,362(14):1282-1291. |
| [14] | Poston L, Briley AL, Seed PT, et al. Vitamin C and vitamin E in pregnant women at risk for pre-eclampsia (VIP trial): randomised placebo-controlled trial[J]. Lancet, 2006,367(9517):1145-1154. |
| [15] |
Rajasingam D, Seed PT, Briley AL, et al. A prospective study of pregnancy outcome and biomarkers of oxidative stress in nulliparous obese women[J]. Am J Obstet Gynecol, 2009,200(4):395.
pmid: 19200933 |
| [16] | 康忠春, 陈远兰, 邹余粮. 妊娠子痫前期孕妇维生素A、E水平及其影响因素分析[J]. 临床医学研究与实践, 2018,3(30):142-144. |
| [17] | 张翠, 靳颖, 杨洁, 等. 河北省产妇2016年妊娠期高血压疾病患病情况分析[J]. 中国公共卫生, 2018,34(10):1395-1397. |
| [18] | 牛影, 徐叶清, 郝加虎, 等. 马鞍山市妇女孕前体质指数和孕期增重与妊娠期高血压疾病的队列研究[J]. 卫生研究, 2016,45(2):205-210. |
| [19] | 申南, 陆娣, 郑春梅, 等. 常规保健下不同年龄段孕妇妊娠早期血清维生素A、E水平分析[J]. 中国妇产科临床杂志, 2018,19(4):356-358. |
| [20] | 闫明, 张雯, 刘凯波, 等. 北京地区2010年—2017年增补叶酸预防神经管缺陷工作效果分析[J]. 中国优生与遗传杂志, 2019,27(3):339-341. |
| [21] | Schiff E, Friedman SA, Stampfer M, et al. Dietary consumption and plasma concentrations of vitamin E in pregnancies complicated by preeclampsia[J]. Am J Obstet Gynecol, 1996,175(4 Pt 1):1024-1028. |
| [22] |
Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies[J]. BMJ, 2016,353:i1753.
pmid: 27094586 |
| [23] | Rumbold AR, Crowther CA, Haslam RR, et al. Vitamins C and E and the risks of preeclampsia and perinatal complications[J]. N Engl J Med, 2006,354(17):1796-1806. |
| [24] | Bowman BA, Russell RM. 现代营养学[M]. 8版. 荫士安,汪之顼, 译. 北京: 化学工业出版社, 2004: 195. |
| [25] | Karpińska J, Mikołuć B, Motkowski R, et al. HPLC method for simultaneous determination of retinol, alpha-tocopherol and coenzyme Q10 in human plasma [J]. J Pharm Biomed Anal, 2006,42(2):232-236. |
| [26] | 马蕊, 刘建蒙, 李松, 等. 浙江省嘉兴地区妊娠高血压综合征发病状况研究[J]. 中华流行病学杂志, 2005,26(12):960-963. |
| [27] | Yusuf H, Subih HS, Obeidat BS, et al. Associations of macro and micronutrients and antioxidants intakes with preeclampsia: A case-control study in Jordanian pregnant women[J]. Nutr Metab Car-diovasc Dis, 2019,29(5):458-466. |
| [28] | 孟凡文, 陈森, 刘亚山, 等. 河北省5县区妊娠期高血压疾病的发病情况及危险因素分析[J]. 中国生育健康杂志, 2015,26(2):112-115. |
| [1] | 马会超,李军,王永清. 妊娠合并炎症性肠病的临床特点[J]. 北京大学学报(医学版), 2024, 56(2): 260-266. |
| [2] | 李洋洋,侯林,马紫君,黄山雅美,刘捷,曾超美,秦炯. 孕期因素与婴儿牛奶蛋白过敏的关系[J]. 北京大学学报(医学版), 2024, 56(1): 144-149. |
| [3] | 刘晓强,周寅. 牙种植同期植骨术围术期高血压的相关危险因素[J]. 北京大学学报(医学版), 2024, 56(1): 93-98. |
| [4] | 游芳凝,罗靓,刘香君,张学武,李春. 未分化结缔组织病患者的妊娠结局、疾病演变及其影响因素[J]. 北京大学学报(医学版), 2023, 55(6): 1045-1052. |
| [5] | 李宇菲,闫亚妮,靳家扬,李春,裴秋艳. 合并胎儿心脏病变的抗SSA抗体阳性孕妇的临床及实验室特征[J]. 北京大学学报(医学版), 2023, 55(6): 1053-1057. |
| [6] | 陈楚云,孙蓬飞,赵静,贾佳,范芳芳,王春燕,李建平,姜一梦,霍勇,张岩. 北京社区人群促红细胞生成素相关因素及其与10年心血管疾病风险的关系[J]. 北京大学学报(医学版), 2023, 55(6): 1068-1073. |
| [7] | 吴洁,张雯,梁舒,秦艺璐,范文强. 妊娠期原发性干燥综合征合并视神经脊髓炎谱系疾病危重症1例[J]. 北京大学学报(医学版), 2023, 55(6): 1118-1124. |
| [8] | 徐金辉,韩娜,苏涛,林力孜,计岳龙,周双,包鹤龄,刘峥,罗树生,徐相蓉,王海俊. 孕早期单纯甲状腺过氧化物酶抗体阳性与胎儿生长的关联[J]. 北京大学学报(医学版), 2023, 55(5): 886-892. |
| [9] | 于欢,杨若彤,王斯悦,吴俊慧,王梦莹,秦雪英,吴涛,陈大方,武轶群,胡永华. 2型糖尿病患者使用二甲双胍与缺血性脑卒中发病风险的队列研究[J]. 北京大学学报(医学版), 2023, 55(3): 456-464. |
| [10] | 孙希雅,陈艺璐,曾琳,闫丽盈,乔杰,李蓉,智旭. 不孕女性维生素D水平与抗苗勒氏管激素的相关性及对妊娠结局的预测[J]. 北京大学学报(医学版), 2023, 55(1): 167-173. |
| [11] | 梁喆,范芳芳,张岩,秦献辉,李建平,霍勇. 中国高血压人群中H型高血压的比率和特征及与美国人群的比较[J]. 北京大学学报(医学版), 2022, 54(5): 1028-1037. |
| [12] | 马麟,吴静依,李双成,李鹏飞,张路霞. 抗高血压药物对二氧化氮长期暴露与慢性肾脏病关联的修饰效应[J]. 北京大学学报(医学版), 2022, 54(5): 1047-1055. |
| [13] | 森本智惠子,王益勤,周蓉,王建六. 子宫内膜非典型增生及子宫内膜癌患者保留生育功能治疗的临床研究[J]. 北京大学学报(医学版), 2022, 54(5): 936-942. |
| [14] | 张红霞,杨蕊,杨硕,潘宁宁,王琳琳,李蓉. 经腹胎儿颅内与胸腔内注射氯化钾减胎的临床效果[J]. 北京大学学报(医学版), 2022, 54(5): 943-947. |
| [15] | 马涛,李艳辉,陈曼曼,马莹,高迪,陈力,马奇,张奕,刘婕妤,王鑫鑫,董彦会,马军. 青春期启动提前与儿童肥胖类型的关联研究: 基于横断面调查和队列调查[J]. 北京大学学报(医学版), 2022, 54(5): 961-970. |
|
||