北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (2): 255-260. doi: 10.19723/j.issn.1671-167X.2021.02.004
血浆Dickkopf-1在类风湿关节炎患者中的表达及其与外周血T细胞亚群的相关性
曹迪1,王燕1,Δ( ),王柳青1,孙晓麟2,黄妃3,孟洋1,任丽丽1,张学武2,Δ(
),王柳青1,孙晓麟2,黄妃3,孟洋1,任丽丽1,张学武2,Δ( )
)
- 1.郑州大学第五附属医院风湿免疫科, 郑州 450000
2.北京大学人民医院风湿免疫科, 北京 100044
3.遵义医科大学附属医院肾病风湿科, 贵州遵义 563000
Expression of plasma Dickkopf-1 in patients with rheumatoid arthritis and its correlation with peripheral blood T cell subsets
CAO Di1,WANG Yan1,Δ( ),WANG Liu-qing1,SUN Xiao-lin2,HUANG Fei3,MENG Yang1,REN Li-li1,ZHANG Xue-wu2,Δ(
),WANG Liu-qing1,SUN Xiao-lin2,HUANG Fei3,MENG Yang1,REN Li-li1,ZHANG Xue-wu2,Δ( )
)
- 1. Department of Rheumatology and Immunology, The Fifth Affiliated Hospital of Zhengzhou University, Zhengzhou 450000, China
2. Department of Rheumatology and Immunology, Peking University People’s Hospital, Beijing 100044, China
3. Department of Rheumatology and Immunology,Affiliated Hospital of Zunyi Medical University, Zunyi 563000, Guizhou, China
摘要:
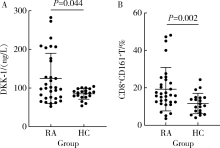
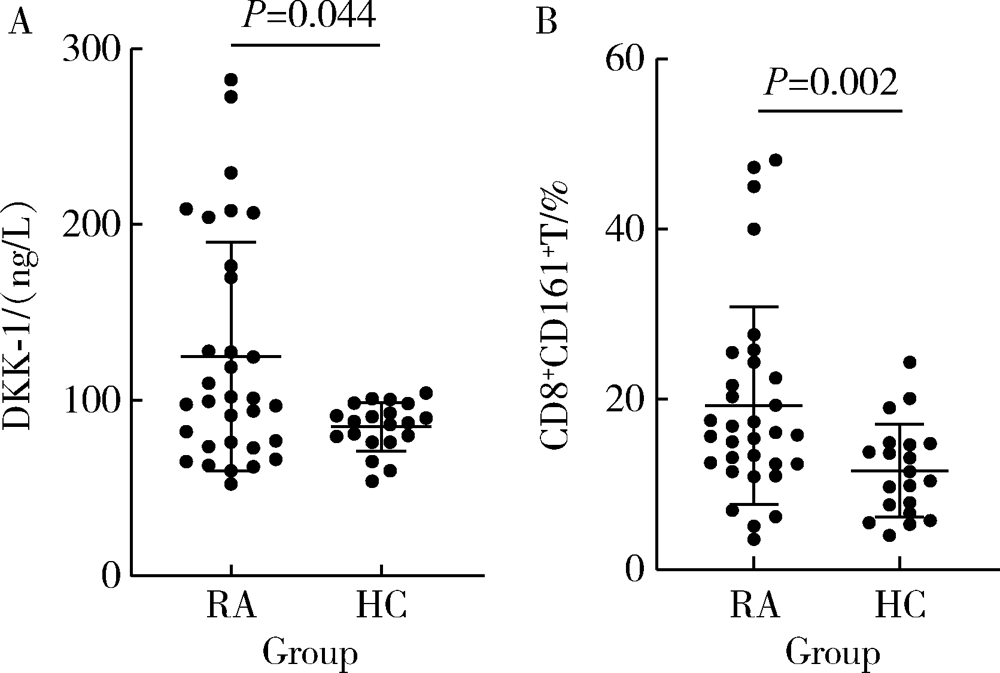
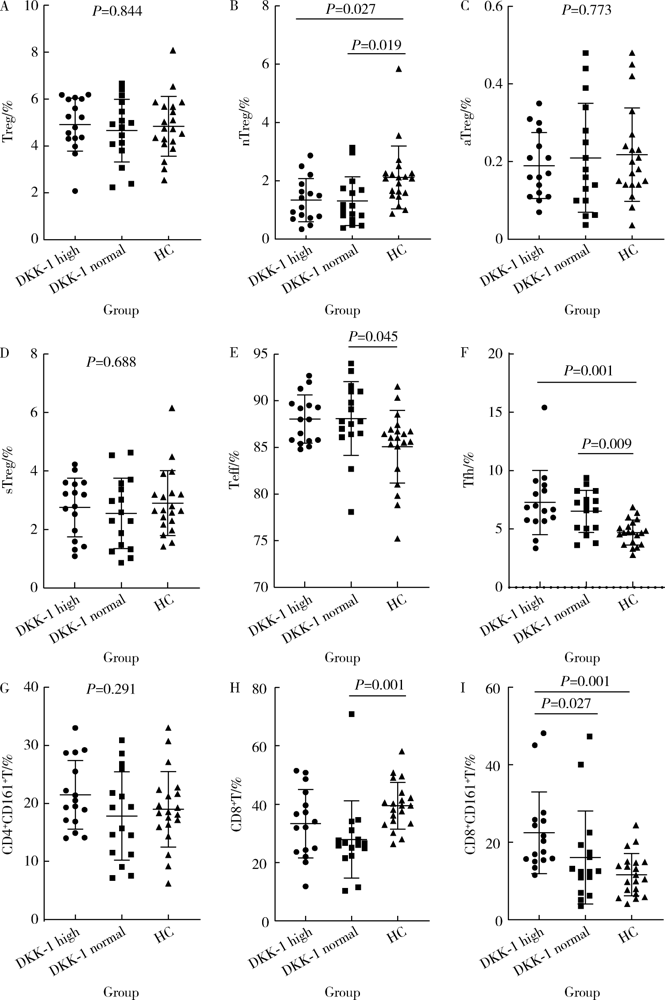
目的: 检测类风湿关节炎(rheumatoid arthritis,RA)患者血浆Dickkopf-1(DKK-1)水平,并分析其与外周血T细胞亚群、临床指标之间的相关性。方法: 采用酶联免疫吸附法(enzyme linked immunosorbent assay,ELISA)检测32例RA患者及20例健康对照者的血浆DKK-1的水平,并记录RA患者的各项临床表现和实验室指标。流式细胞仪检测RA患者外周血T细胞亚群(包括Treg、nTreg、aTreg、sTreg、Teff、Tfh、CD4+CD161+T、CD8+T、CD8+CD161+T细胞)。比较两组血浆DKK-1的水平,并分析其与外周血T细胞亚群、临床指标的相关性。结果: (1)RA患者血浆DKK-1浓度为(124.97±64.98) ng/L,健康对照组血浆DKK-1浓度为(84.95±13.74) ng/L,RA患者血浆DKK-1水平显著高于健康对照组(P<0.05),RA患者外周血CD8+CD161+T细胞百分比显著高于健康对照组(P<0.05)。(2)血浆DKK-1水平与红细胞沉降率(r=0.406,P=0.021)、DAS28评分(r=0.372,P=0.036)、免疫球蛋白G(r=0.362,P=0.042)、免疫球蛋白A(r=0.377,P=0.033)呈正相关;与年龄、病程、C-反应蛋白、类风湿因子、抗环瓜氨酸肽抗体、免疫球蛋白M、补体C3、补体C4、白细胞计数、中性粒细胞百分比无相关性。(3)RA患者血浆DKK-1水平与外周血CD8+CD161+T细胞百分比呈正相关(r=0.413,P=0.019);与Treg、nTreg、aTreg、sTreg、Teff、Tfh、CD4+CD161+T、CD8+T细胞无相关性。(4)外周血CD161+CD8+T细胞百分比与红细胞沉降率(r=-0.415,P=0.004)、C-反应蛋白(r=-0.393,P=0.007)、DAS28评分(r=-0.392,P=0.007)、类风湿因子(r=-0.535,P<0.001)、抗环瓜氨酸肽抗体(r=-0.589,P<0.001)、免疫球蛋白G(r=-0.368,P=0.012)、免疫球蛋白M(r=-0.311,P=0.035)呈负相关;与年龄、病程、免疫球蛋白A、补体C3、补体C4、白细胞计数、中性粒细胞百分比无相关性。结论: RA患者血浆DKK-1水平和外周血T细胞亚群中的CD8+CD161+T细胞百分比均升高,可能与患者体内促炎细胞因子的分泌有关;DKK-1参与骨稳态的调节,可用作RA骨破坏的标志物。
中图分类号:
- R593.2
| [1] |
Smolen JS, Aletaha D, Mcinnes IB. Rheumatoid arthritis[J]. Lancet, 2016,388(10055):2023-2038.
pmid: 27156434 |
| [2] | Lee GR. The balance of Th17 versus Treg cells in autoimmunity[J]. Int J Mol Sci, 2018,19(3):730. |
| [3] |
Chae WJ, Park JH, Henegariu O, et al. Membrane-bound Dickkopf-1 in Foxp3+ regulatory T cells suppresses T-cell-mediated autoimmune colitis[J]. Immunology, 2017,152(2):265-275.
pmid: 28556921 |
| [4] |
Chae WJ, Ehrlich AK, Chan PY, et al. The Wnt antagonist Dickkopf-1 promotes pathological type 2 cell-mediated Inflammation[J]. Immunity, 2016,44(2):246-258.
pmid: 26872695 |
| [5] | Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative[J]. Ann Rheum Dis, 2010,62(9):2569-2581. |
| [6] |
Glinka A, Wu W, Delius H, et al. Dickkopf-1 is a member of a new family of secreted proteins and functions in head induction[J]. Nature, 1998,391(6665):357-362.
pmid: 9450748 |
| [7] | Fujita K, Janz S. Attenuation of WNT signaling by DKK-1 and -2 regulates BMP2-induced osteoblast differentiation and expression of OPG, RANKL and M-CSF[J]. Mol Cancer, 2007,6(1):71. |
| [8] |
Diarra D, Stolina M, Polzer K, et al. Dickkopf-1 is a master regulator of joint remodeling[J]. Nat Med, 2007,13(2):156-163.
pmid: 17237793 |
| [9] | Gómez-Vaquero C, Martín I, Loza E, et al. Effect of osteoprotegerin and Dickkopf-related protein 1 on radiological progression in tightly controlled rheumatoid arthritis[J]. PLoS One, 2016,11(12):e0166691. |
| [10] |
Rout N. Enhanced Th1/Th17 functions of CD161+CD8+T cells in mucosal tissues of rhesus macaques[J]. PLoS One, 2016,11(6):e0157407.
pmid: 27309719 |
| [11] | Mitsuo A, Morimoto S, Nakiri Y, et al. Decreased CD161+CD8+ T cells in the peripheral blood of patients suffering from rheumatic diseases[J]. Rheumatology (Oxford), 2006,45(12):1477-1484. |
| [12] |
Nicol B, Salou M, Vogel I, et al. An intermediate level of CD161 expression defines a novel activated, inflammatory, and pathogenic subset of CD8+T cells involved in multiple sclerosis[J]. J Autoimmun, 2018,88:61-74.
doi: 10.1016/j.jaut.2017.10.005 |
| [1] | 刘东武, 陈杰, 高明利, 于静. 类风湿关节炎伴发淋巴结Castleman样病理改变1例[J]. 北京大学学报(医学版), 2024, 56(5): 928-931. |
| [2] | 黄会娜,赵静,赵祥格,白自然,李霞,王冠. 乳酸对类风湿关节炎患者外周血CD4+T细胞亚群的调控作用[J]. 北京大学学报(医学版), 2024, 56(3): 519-525. |
| [3] | 汤晓菲,李永红,丁秋玲,孙卓,张阳,王育梅,田美伊,刘坚. 类风湿关节炎患者下肢深静脉血栓发病率及危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 279-283. |
| [4] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [5] | 扶琼,叶霜. 嵌合抗原受体T细胞治疗在自身免疫疾病中的应用和思考[J]. 北京大学学报(医学版), 2023, 55(6): 953-957. |
| [6] | 吴琦,蔡月明,何娟,黄文蒂,王庆文. 血脂异常与类风湿关节炎肺间质病变的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 982-992. |
| [7] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 体重指数与类风湿关节炎临床特征的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 993-999. |
| [8] | 金银姬,孙琳,赵金霞,刘湘源. 血清IgA型抗鼠科肉瘤病毒癌基因同源物B1抗体在类风湿关节炎中的意义[J]. 北京大学学报(医学版), 2023, 55(4): 631-635. |
| [9] | 时云飞,王豪杰,刘卫平,米岚,龙孟平,刘雁飞,赖玉梅,周立新,刁新婷,李向红. 血管免疫母细胞性T细胞淋巴瘤临床与分子病理学特征分析[J]. 北京大学学报(医学版), 2023, 55(3): 521-529. |
| [10] | 蔡文心,李仕成,刘一鸣,梁如玉,李静,郭建萍,胡凡磊,孙晓麟,李春,刘栩,叶华,邓立宗,李茹,栗占国. 类风湿关节炎临床分层及其特征的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1068-1073. |
| [11] | 程昉,杨邵英,房星星,王璇,赵福涛. CCL28-CCR10通路在类风湿关节炎单核细胞迁移中的作用[J]. 北京大学学报(医学版), 2022, 54(6): 1074-1078. |
| [12] | 刘蕊,赵金霞,闫良. 类风湿关节炎合并下肢静脉血栓患者的临床特点[J]. 北京大学学报(医学版), 2022, 54(6): 1079-1085. |
| [13] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 类风湿关节炎患者生活质量与疾病活动度的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1086-1093. |
| [14] | 程晓静,蒋栋,张连海,王江华,李雅真,翟佳慧,闫宝琪,张露露,谢兴旺,李子禹,季加孚. KRAS G12V特异性T细胞受体治疗恶性肿瘤的临床前研究[J]. 北京大学学报(医学版), 2022, 54(5): 884-895. |
| [15] | 高超,陈立红,王莉,姚鸿,黄晓玮,贾语博,刘田. 类风湿关节炎合并纤维肌痛简易分类标准的临床验证[J]. 北京大学学报(医学版), 2022, 54(2): 278-282. |
|
||