北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 865-870. doi: 10.19723/j.issn.1671-167X.2021.05.009
前交叉韧带重建术后移植物应力的有限元分析
任爽,时会娟,张家豪,刘振龙,邵嘉艺,朱敬先,胡晓青,黄红拾,敖英芳( )
)
- 北京大学第三医院运动医学科,北京大学运动医学研究所,运动医学关节伤病北京市重点实验室,北京 100191
Finite element analysis of the graft stresses after anterior cruciate ligament reconstruction
REN Shuang,SHI Hui-juan,ZHANG Jia-hao,LIU Zhen-long,SHAO Jia-yi,ZHU Jing-xian,HU Xiao-qing,HUANG Hong-shi,AO Ying-fang( )
)
- Beijing Key Laboratory of Sports Injuries, Beijing 100191, China
摘要:
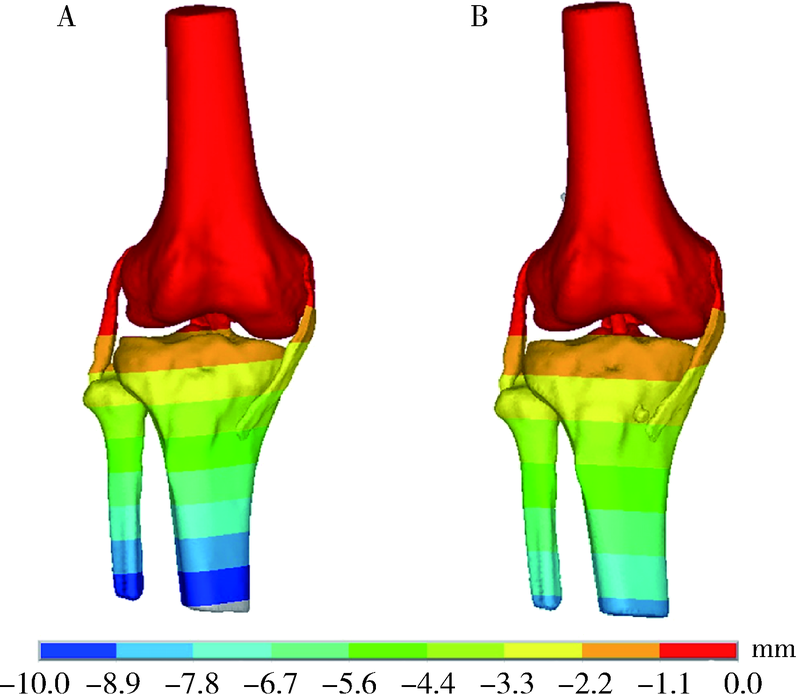
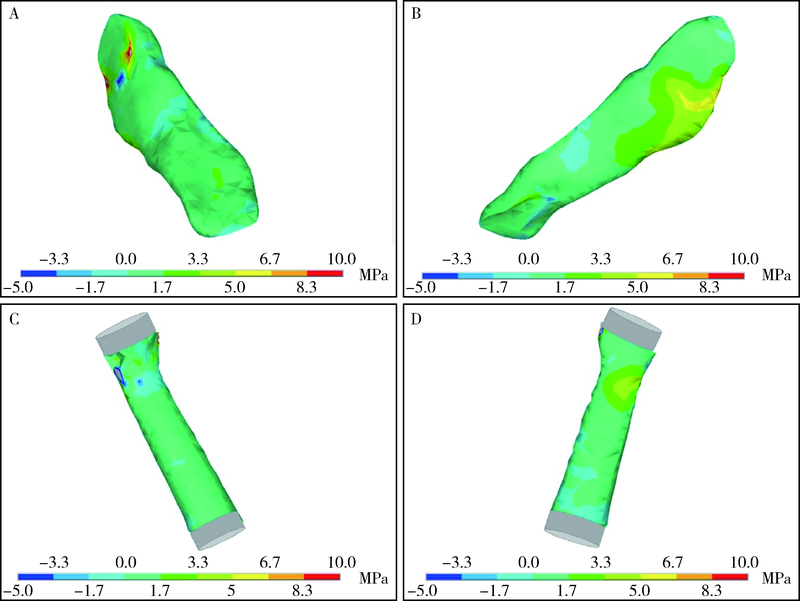
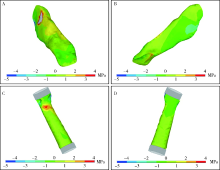
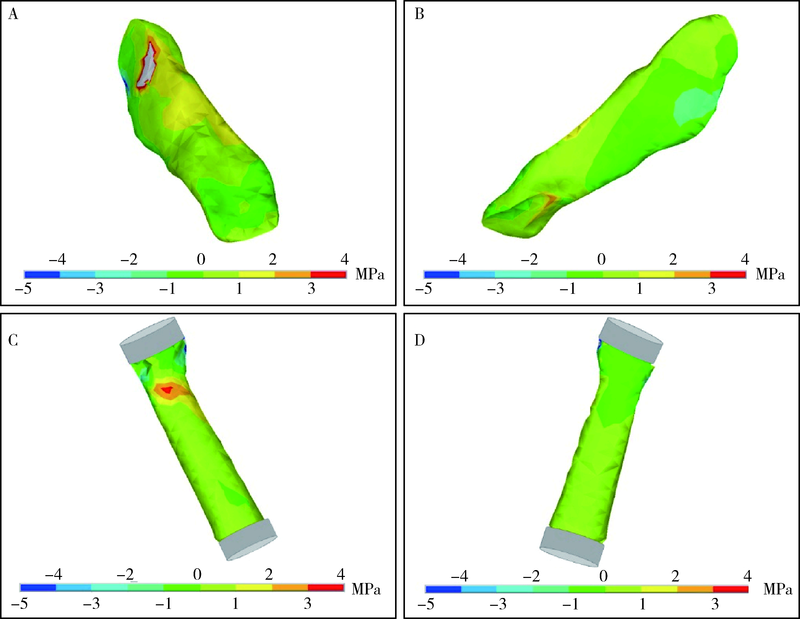
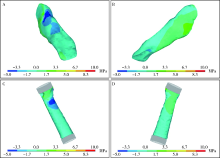
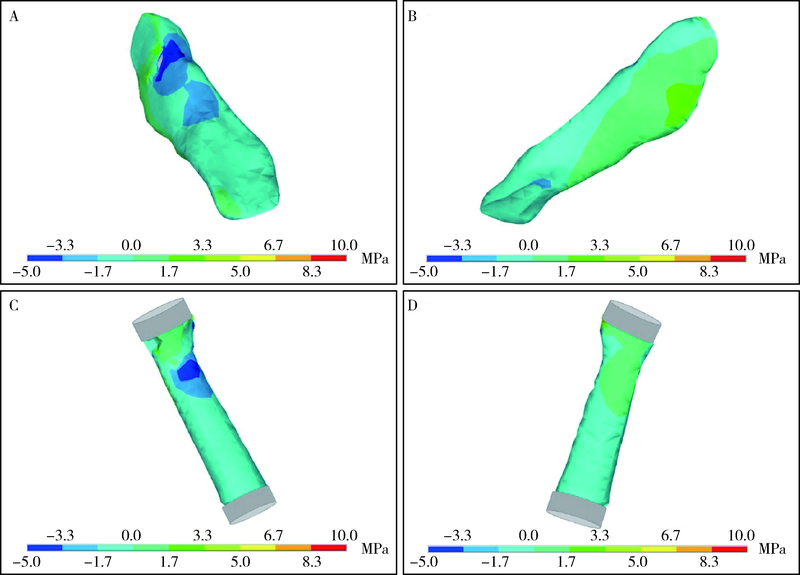
目的: 探究前交叉韧带(anterior cruciate ligament, ACL)重建后移植物应力分布特征,为ACL重建的手术方案提供理论参考。方法: 基于三维磁共振及CT影像,建立完整膝关节有限元模型,模型包括股骨、胫骨、腓骨、内侧副韧带、外侧副韧带、ACL、后交叉韧带;建立ACL重建后膝关节有限元模型,模型包括股骨、胫骨、腓骨、内侧副韧带、外侧副韧带、ACL移植物、后交叉韧带。模型采用线弹性材料属性,骨组织材料属性设置为弹性模量17 GPa,泊松比(Poisson’s ratio)为0.36;完整膝关节及ACL重建膝关节的模型中的韧带组织及ACL移植物的材料属性设置为弹性模量390 MPa,泊松比0.4;将股骨固定设置为模型边界条件,施加胫骨前向134 N的拉力为载荷条件,求解分析完整膝关节的ACL及重建术后的ACL移植物的拉应力、压应力、剪切应力、等效应力的受力状态。结果: 重建后的ACL移植物的最大压应力(6.34 MPa)、等效应力(5.9 MPa)、剪切应力(1.83 MPa)均在前侧股骨端,与完整膝关节ACL最大压应力(8.77 MPa)、等效应力(8.88 MPa)、剪切应力(3.44 MPa)位置一致。移植物最大拉应力也出现在股骨端,但位置在后侧,与完整膝关节ACL最大拉应力位置一致,且ACL移植物最大拉应力的值仅为0.88 MPa,小于完整膝关节ACL的2.56 MPa。结论: ACL移植物压应力、等效应力、剪切应力最大值均在前侧股骨端,最大拉应力出现在股骨端后侧,均与完整膝关节ACL最大拉应力位置一致;ACL移植物的前侧部分承受力较大,后侧部分承受力较小,与ACL的生物力学特性相符合。
中图分类号:
- R686.5
| [1] |
Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: A 10-year study [J]. Knee, 2006, 13(3):184-188.
pmid: 16603363 |
| [2] |
DePhillipo NN, Moatshe G, Brady A, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: A biomechanical study [J]. Am J Sports Med, 2018, 46(10):2422-2431.
doi: 10.1177/0363546518774315 pmid: 29847148 |
| [3] | 时会娟, 丁立, 任爽, 等. 前交叉韧带重建术后步行过程中的生物力学特征 [J]. 科技导报, 2020, 38(6):25-33. |
| [4] | 杨骁, 李彦林, 刘德建, 等. 三维有限元分析在前交叉韧带重建中的应用研究进展 [J]. 中国运动医学杂志, 2020, 39(9):742-745. |
| [5] |
Vairis A, Stefanoudakis G, Petousis M, et al. Evaluation of an intact, an ACL-deficient, and a reconstructed human knee joint finite element model [J]. Comput Methods Biomech Biomed Engin, 2016, 19(3):263-270.
doi: 10.1080/10255842.2015.1015526 |
| [6] |
Butler DL, Guan Y, Kay MD, et al. Location-dependent variations in the material properties of the anterior cruciate ligament [J]. J Biomech, 1992, 25(5):511-518.
pmid: 1592856 |
| [7] |
Ng GY, Oakes BW, Deacon OW, et al. Biomechanics of patellar tendon autograft for reconstruction of the anterior cruciate ligament in the goat: Three-year study [J]. J Orthop Res, 1995, 13(4):602-608.
pmid: 7674076 |
| [8] |
Gali JC, Camargo DB, Oliveira FAM, et al. Anatomia descritiva da inserção femoral do ligamento cruzado anterior [J]. Rev Bras Ortop, 2018, 53(4):421-426.
doi: 10.1016/j.rbo.2017.03.003 |
| [9] |
Scheffler SU, Maschewski K, Becker R, et al. In-vivo three-dimensional MR imaging of the intact anterior cruciate ligament shows a variable insertion pattern of the femoral and tibial footprints [J]. Knee Surg Sports Traumatol Arthrosc, 2018, 26(12):3667-3672.
doi: 10.1007/s00167-018-4939-x |
| [10] | 汪田福, 郝智秀, 高相飞. 前交叉韧带生物力学特性及其损伤对膝关节稳定性的影响 [J]. 清华大学学报(自然科学版), 2010, 50(7):1005-1008. |
| [11] |
Fox R, Harner C, Sakane M, et al. Determination of the in situ forces in the human posterior cruciate ligament using robotic technology: A cadaveric study [J]. Am J Sports Med, 1998, 26(3):395-401.
doi: 10.1177/03635465980260030901 |
| [12] |
Peña E, Calvo B, Martínez MA, et al. A three-dimensional finite element analysis of the combined behavior of ligaments and menisci in the healthy human knee joint [J]. J Biomech, 2006, 39(9):1686-1701.
pmid: 15993414 |
| [13] |
Tampere T, Devriendt W, Cromheecke M, et al. Tunnel placement in ACL reconstruction surgery: Smaller inter-tunnel angles and higher peak forces at the femoral tunnel using anteromedial portal femoral drilling: A 3D and finite element analysis [J]. Knee Surg Sports Traumatol Arthrosc, 2019, 27(8):2568-2576.
doi: 10.1007/s00167-018-5272-0 |
| [14] |
Salehghaffari S, Dhaher YY. A model of anterior cruciate ligament reconstructive surgery: A validation construct and computational insights [J]. J Biomech, 2014, 47(7):1609-1617.
doi: 10.1016/j.jbiomech.2014.03.003 pmid: 24690279 |
| [15] |
van der Bracht H, Tampere T, Beekman P, et al. Peak stresses shift from femoral tunnel aperture to tibial tunnel aperture in lateral tibial tunnel ACL reconstructions: A 3D graft-bending angle measurement and finite-element analysis [J]. Knee Surg Sports Traumatol Arthrosc, 2018, 26(2):508-517.
doi: 10.1007/s00167-017-4739-8 |
| [1] | 任爽, 时会娟, 梁子轩, 张思, 胡晓青, 黄红拾, 敖英芳. 前交叉韧带重建术后侧切动作的生物力学特征[J]. 北京大学学报(医学版), 2024, 56(5): 868-873. |
| [2] | 王江静,魏顺依,敖英芳,杨渝平. 前交叉韧带重建术后三种不同药物镇痛早期疗效的对比[J]. 北京大学学报(医学版), 2024, 56(2): 293-298. |
| [3] | 欧蒙恩,丁云,唐卫峰,周永胜. 基台边缘-牙冠的平台转移结构中粘接剂流动的三维有限元分析[J]. 北京大学学报(医学版), 2023, 55(3): 548-552. |
| [4] | 马珂楠,陈虎,沈妍汝,周永胜,王勇,孙玉春. 选择性激光熔化打印可摘局部义齿圆环形卡环固位力的有限元分析[J]. 北京大学学报(医学版), 2022, 54(1): 105-112. |
| [5] | 印钰,梅宇,王泽刚,宋首一,刘鹏飞,何鹏峰,武文杰,谢兴. 固定袢和可调节袢在粗骨道中的长度对股骨骨道增宽及膝关节功能的影响[J]. 北京大学学报(医学版), 2021, 53(5): 883-890. |
| [6] | 蒋艳芳,王健,王永健,刘佳,裴殷,刘晓鹏,敖英芳,马勇. 前交叉韧带翻修重建术后中长期临床疗效及影响因素[J]. 北京大学学报(医学版), 2021, 53(5): 857-863. |
| [7] | 周伟,安金刚,荣起国,张益. 下颌骨颏部骨折联合双侧髁突囊内骨折致伤机制的三维有限元分析[J]. 北京大学学报(医学版), 2021, 53(5): 983-989. |
| [8] | 姜又升,冯琳,高学军. 垫底材料弹性模量对髓腔固位冠修复后上颌前磨牙应力分布的影响[J]. 北京大学学报(医学版), 2021, 53(4): 764-769. |
| [9] | 林春平,卢松鹤,朱浚鑫,胡洪成,岳兆国,唐志辉. 个性化根形种植体的螺纹形态对周围牙槽骨应力分布影响的三维有限元分析[J]. 北京大学学报(医学版), 2019, 51(6): 1130-1137. |
| [10] | 张家豪,任爽,邵嘉艺,牛星跃,胡晓青,敖英芳. 前交叉韧带生物力学止点重建的解剖学与有限元分析[J]. 北京大学学报(医学版), 2019, 51(3): 586-590. |
| [11] | 付宏宇,王芳芳,侯晓玫. 控制记忆合金丝镍钛根管锉弯曲性能有限元分析模型的构建及力学分析[J]. 北京大学学报(医学版), 2019, 51(1): 131-135. |
| [12] | 柳大为,李晶,郭亮,荣起国,周彦恒. 舌侧矫治器关闭间隙上前牙牙周膜应力变化的三维有限元分析[J]. 北京大学学报(医学版), 2018, 50(1): 141-147. |
| [13] | 孙丽颖,郭阳,荣起国,田光磊. 舟骨骨折术后康复治疗的有限元分析[J]. 北京大学学报(医学版), 2016, 48(4): 751-封三. |
| [14] | 赵旭, 张磊, 孙健, 杨振宇,谢秋菲. 后牙种植体支持单冠牙合面高度的三维有限元力学分析[J]. 北京大学学报(医学版), 2016, 48(1): 94-100. |
| [15] | 甄敏,胡文杰,荣起国. 上颌中切牙冠根折行冠延长术并桩核冠修复的三维有限元分析[J]. 北京大学学报(医学版), 2015, 47(6): 1015-1021. |
|
||