北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 970-976. doi: 10.19723/j.issn.1671-167X.2021.05.027
后牙区单牙种植修复5年后的临床修复疗效观察
- 北京大学口腔医学院·口腔医院,第二门诊部 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100101
Clinical observation of the curative effect after 5-year follow-up of single tooth implant-supported restorations in the posterior region
LIANG Feng,WU Min-jie( ),ZOU Li-dong
),ZOU Li-dong
- Second Clinical Division, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100101, China
摘要:
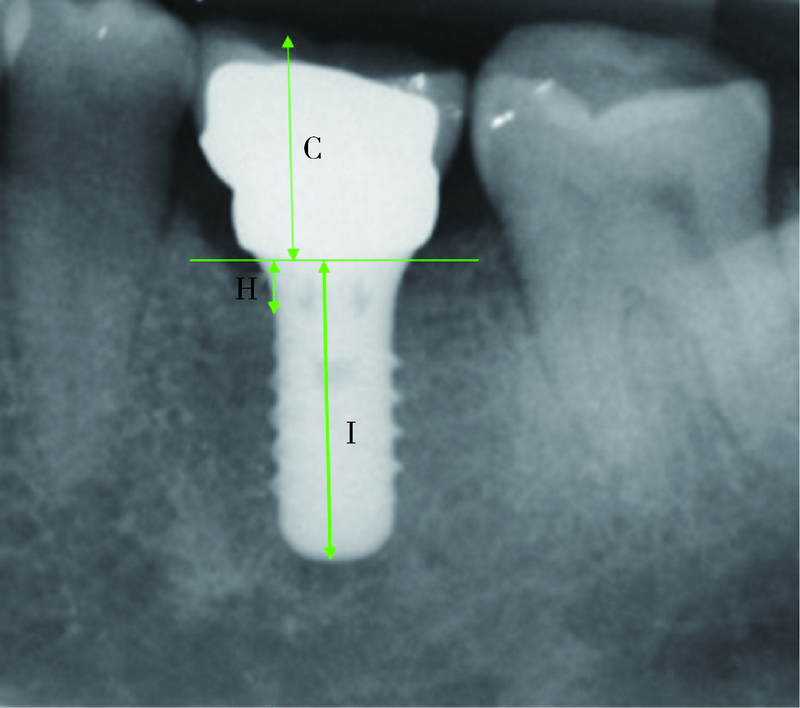
目的: 分析后牙区单牙种植修复患者在行使功能5年后的临床修复疗效。方法: 选取2005年10月至2010年5月在北京大学口腔医院第二门诊部接受种植治疗并且负重已达到5年的后牙区种植治疗患者,回顾患者的临床资料、X线片、种植体近远中边缘骨高度的变化以及修复体的情况(包括修复体完整性、松动情况、螺丝孔封闭材料存留状况、修复体固位螺丝及修复基台的松动或折断情况)来评估临床疗效。结果: 215例患者,平均年龄48.6岁(27~71岁),共植入软组织水平种植体321枚(其中上颌126枚、下颌195枚)。9枚种植体在回访期间出现松动、脱落,累计存留率达97.2%。存留的312枚种植体中,上颌120枚、下颌192枚,其中直径为3.3、4.1和4.8 mm的种植体分别为5枚(1.6%)、115枚(36.9%)和192枚(61.5%),长度为8、10和12 mm的种植体分别为21枚(6.7%)、206枚(66.0%)和85枚(27.2%)。上部修复体固位方式中,粘接固位为277枚(88.8%),螺丝固位为35枚(11.2%)。负载5年后种植体近远中牙槽骨高度平均吸收分别为(0.73±0.25) mm和(0.78±0.26) mm,近远中骨吸收程度与植入区骨质类型、种植体规格、修复基台角度、固位方式、临床冠-种植体长度比、性别、年龄等因素均未显示有相关性(P>0.05)。修复后主要的机械并发症有:修复体固位螺丝松动(8.6%)或折断(2.9%)、修复体上螺丝孔封闭材料脱落(11.4%)、修复体崩瓷(13.8%)及修复体脱粘(14.1%),其中仅修复体脱粘的发生率与修复时使用的基台角度(0°/15°)和修复体的临床高度这两个因素相关(P<0.05)。结论: 软组织水平种植体在单颗后牙缺失的修复病例中负重5年后,种植体周围的骨水平基本稳定,全面完善的种植诊疗计划、规范严谨的临床操作以及定期的复查可能是减少修复后并发症的有效方法。
中图分类号:
- R783.6
| [1] |
Jung RE, Pjetrusson BE, Glauser R, et al. A systematic review of the 5-year survival and complication rates of implant-supported single crowns [J]. Clin Oral Implants Res, 2008, 19(2):119-130.
doi: 10.1111/clr.2008.19.issue-2 |
| [2] | Pjetursson BE, Thoma D, Jung R, et al. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years [J]. Clin Oral Implants Res, 2012, 23(Suppl 6):22-38. |
| [3] | Zembic A, Kim S, Zwahlen M, et al. Systematic review of the survival rate and incidence of biologic, technical, and esthetic complications of single implant abutments supporting fixed prostheses [J]. Int J Oral Maxillofac Implants, 2014, 29(Suppl):99-116. |
| [4] | Hjalmarsson L, Gheisarifar M, Jemt T. A systematic review of survival of single implants as presented in longitudinal studies with a follow-up of at least 10 years [J]. I Eur J Oral Implantol, 2016, 9(Suppl 1):S155-162. |
| [5] | Garlini G, Chierichetti V, D’Amato S, et al. A long term follow-up of single-tooth Xive implant: 15 year results [J]. Dent Oral Craniofac Res, 2016, 3(1):1-4. |
| [6] |
Arunyanak SP, Pollini A, Ntounis A, et al. Clinician assessments and patient perspectives of single-tooth implant restorations in the esthetic zone of the maxilla: A systematic review [J]. J Prosthet Dent, 2017, 118(1):10-17.
doi: S0022-3913(16)30691-6 pmid: 28385430 |
| [7] |
Chrcanovic BR, Kisch J, Larsson C. Retrospective clinical evaluation of implant-supported single crowns: Mean follow-up of 15 years [J]. Clin Oral Implants Res, 2019, 30(7):691-701
doi: 10.1111/clr.2019.30.issue-7 |
| [8] | 林野, 李健慧, 邱立新, 等. 口腔种植修复临床效果十年回顾研究 [J]. 中华口腔医学杂志, 2006, 41(3):131-135. |
| [9] | 朱艳香, 程然, 林梓桐, 等. 上颌后牙区种植修复后6~9年临床疗效观察 [J]. 东南大学学报(医学版), 2017, 36(5):841-846. |
| [10] | 张燕婷, 李悦, 何晶, 等. 上颌后牙区不同术式种植修复10年累计存留率及患者相关因素对其成功率的影响分析 [J]. 中国实用口腔科杂志, 2017, 10(1):31-35. |
| [11] | Wheeler SL, Holmes RE, Calhoun CJ. Six-year clinical and histologic study of sinus-lift grafts [J]. Int J Oral Maxillofac Implants, 1996, 11(1):26-34. |
| [12] |
Renouard F, Nisand D. Impact of implant length and diameter on survival rates [J]. Clin Oral Implants Res, 2006, 17(Suppl 2):35-51.
doi: 10.1111/clr.2006.17.issue-s2 |
| [13] |
Zimmermann J, Sommer M, Grize L, et al. Marginal bone loss 1 year after implantation: a systematic review for fixed and removable restorations [J]. Clin Cosmet Investig Dent, 2019, 11:195-218.
doi: 10.2147/CCIDE |
| [14] | Pellicer-Chover H, Díaz-Sanchez M, Soto-Penaloza D, et al. Impact of crestal and subcrestal implant placement upon changes in marginal peri-implant bone level: A systematic review [J]. Med Oral Patol Oral Cir Bucal, 2019, 24(5):673-683. |
| [15] | Galindo-Moreno P, León-Cano A, Ortega-Oller I, et al. Marginal bone loss as success criterion in implant dentistry: beyond 2 mm [J]. Clin Oral Implants Res, 2015, 26(4):28-34. |
| [1] | 王聪伟,高敏,于尧,章文博,彭歆. 游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析[J]. 北京大学学报(医学版), 2024, 56(1): 66-73. |
| [2] | 李穗,马雯洁,王时敏,丁茜,孙瑶,张磊. 上前牙种植单冠修复体切导的数字化设计正确度[J]. 北京大学学报(医学版), 2024, 56(1): 81-87. |
| [3] | 丁茜,李文锦,孙丰博,谷景华,林元华,张磊. 表面处理对氧化钇和氧化镁稳定的氧化锆种植体晶相及断裂强度的影响[J]. 北京大学学报(医学版), 2023, 55(4): 721-728. |
| [4] | 欧蒙恩,丁云,唐卫峰,周永胜. 基台边缘-牙冠的平台转移结构中粘接剂流动的三维有限元分析[J]. 北京大学学报(医学版), 2023, 55(3): 548-552. |
| [5] | 孙菲,刘建,李思琪,危伊萍,胡文杰,王翠. 种植体黏膜下微生物在健康种植体和种植体周炎中的构成与差异:一项横断面研究[J]. 北京大学学报(医学版), 2023, 55(1): 30-37. |
| [6] | 王鹃,尉华杰,孙井德,邱立新. 预成刚性连接杆用于无牙颌种植即刻印模制取的应用评价[J]. 北京大学学报(医学版), 2022, 54(1): 187-192. |
| [7] | 李琳琳,赵一姣,陈虎,王勇,孙玉春. 转移牙合架固定法三维重建牙尖交错牙合的精度评价[J]. 北京大学学报(医学版), 2020, 52(1): 138-143. |
| [8] | 释栋,曹婕,戴世爱,孟焕新. 植体周炎再生治疗短期疗效观察[J]. 北京大学学报(医学版), 2020, 52(1): 58-63. |
| [9] | 罗强,丁茜,张磊,谢秋菲. 后牙种植冠桥修复后局部咬合变化的定量分析[J]. 北京大学学报(医学版), 2019, 51(6): 1119-1123. |
| [10] | 林春平,卢松鹤,朱浚鑫,胡洪成,岳兆国,唐志辉. 个性化根形种植体的螺纹形态对周围牙槽骨应力分布影响的三维有限元分析[J]. 北京大学学报(医学版), 2019, 51(6): 1130-1137. |
| [11] | 刘潇倩,陈秋雯,冯海兰,王兵,屈健,孙振,衡墨迪,潘韶霞. 无牙颌患者locator附着体种植覆盖义齿修复后口腔卫生维护的纵向研究[J]. 北京大学学报(医学版), 2019, 51(1): 136-144. |
| [12] | 吴敏节,邹立东,梁峰. 上前牙即刻种植即刻修复负载3年后软、硬组织变化的临床观察[J]. 北京大学学报(医学版), 2018, 50(4): 694-699. |
| [13] | 刘婧寅,陈飞,葛严军,魏菱,潘韶霞,冯海兰. 选择性激光熔化种植体对早期骨矿化沉积率的影响[J]. 北京大学学报(医学版), 2018, 50(1): 117-122. |
| [14] | 梁乃文,石磊,黄颖,邓旭亮. 不同形貌纯钛表面对人脐静脉内皮细胞生物学行为的影响[J]. 北京大学学报(医学版), 2017, 49(1): 43-048. |
| [15] | 赵丽萍, 詹雅琳, 胡文杰, 王浩杰, 危伊萍, 甄敏, 徐涛, 刘云松. 磨牙位点保存后进行种植修复及软组织增量的1例报告[J]. 北京大学学报(医学版), 2016, 48(6): 1090-1094. |
|
||