北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (4): 680-685. doi: 10.19723/j.issn.1671-167X.2022.04.016
多原发癌合并肾癌的治疗及预后
邱敏1,连岩岩2,陆敏3,王滨帅1,田晓军1,卢剑1,刘承1,*( ),张树栋1,姜敏4,马潞林1,*(
),张树栋1,姜敏4,马潞林1,*( )
)
- 1. 北京大学第三医院泌尿外科,北京 100191
2. 北京中医药大学第三临床医学院,北京 100029
3. 北京大学第三医院病理科,北京 100191
4. 北京中医药大学东方医院肿瘤科,北京 100078
Treatment and prognosis of multiple primary malignant neoplasms complicated with renal cell carcinoma
Min QIU1,Yan-yan LIAN2,Min LU3,Bin-shuai WANG1,Xiao-jun TIAN1,Jian LU1,Cheng LIU1,*( ),Shu-dong ZHANG1,Min JIANG4,Lu-lin MA1,*(
),Shu-dong ZHANG1,Min JIANG4,Lu-lin MA1,*( )
)
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. The Third Clinical Medical College of Beijing University of Chinese Medicine, Beijing 100029, China
3. Department of Pathology, Peking University Third Hospital, Beijing 100191, China
4. Department of Oncology, Dong Fang Hospital of Beijing University of Chinese Medicine, Beijing 100078, China
摘要:
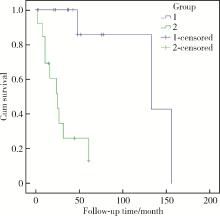
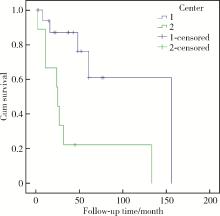
目的: 探讨多原发癌合并肾癌的治疗及预后,并进行风险分层。方法: 回顾性研究两个中心的27例多原发癌合并肾癌资料,包括多原发癌的病种及具体治疗方法、各原发癌的间隔时间等,同时随访生存情况,包括复发、转移及存活情况,进行统计学分析。其中两种原发癌的间隔时间在6个月以内为同时性多原发癌,6个月以上为异时性多原发癌。对病例进行简单的风险分层:多原发癌中只要有一种恶性肿瘤分期在Ⅲ期及以上者定义为高风险,否则为低风险。结果: 本组27例患者中,男20例,女7例。第一原发癌(首发癌)年龄42~82岁,平均(61.3±11.7)岁;发现肾癌时年龄43~87岁,平均(66.0±11.3)岁。首发癌与第二原发癌中位间隔时间18个月(0~360个月)。27例患者中二重癌21例,三重癌4例,四重癌2例;异时性多原发癌17例,同时性多原发癌10例。肾癌合并的多原发癌中以累及泌尿系统、消化系统和呼吸系统最为常见,具体为膀胱癌、肺癌、结肠癌。从最后一种原发癌开始计算的中位随访时间为32个月(2~156个月),有14例存活,死亡的13例中有11例与肿瘤相关。肿瘤分期是预后的影响因素,有一种肿瘤分期在Ⅲ期及以上者(高风险组)预后相对较差。结论: 多原发癌合并肾癌相对少见,治疗过程中应对各肿瘤进行标准化治疗,预后主要取决于各肿瘤中分期最高者,简单风险分层显示高风险组预后更差,此种分层方法可能对预测预后有一定帮助。
中图分类号:
- R737.11
| 1 |
Matzkin H , Braf Z . Multiple primary malignant neoplasms in the genitourinary tract: Occurrence and etiology[J]. J Urol, 1989, 142 (1): 1- 12.
doi: 10.1016/S0022-5347(17)38649-4 |
| 2 |
宋航, 邱敏, 卢剑, 等. 合并肾癌的多原发癌诊断与治疗[J]. 北京大学学报(医学版), 2016, 48 (5): 926- 929.
doi: 10.3969/j.issn.1671-167X.2016.05.034 |
| 3 | Warren S , Gates O . Multiple primary malignant tumor A surgery of the literature and statistical study[J]. Am J Cancer, 1932, 51 (16): 1358- 1414. |
| 4 |
Moertel CG , Dockerty MB , Baggenstoss AH . Multiple primary malignant neoplasms. Ⅰ. Introduction and presentation of data[J]. Cancer, 1961, 14, 221- 230.
doi: 10.1002/1097-0142(196103/04)14:2<221::AID-CNCR2820140202>3.0.CO;2-6 |
| 5 |
Feller A , Matthes KL , Bordoni A , et al. The relative risk of second primary cancers in Switzerland: A population-based retrospective cohort study[J]. BMC Cancer, 2020, 20 (1): 51- 65.
doi: 10.1186/s12885-019-6452-0 |
| 6 |
Tanjak P , Suktitipat B , Vorasan N , et al. Risks and cancer associations of metachronous and synchronous multiple primary can-cers: A 25-year retrospective study[J]. BMC Cancer, 2021, 21 (1): 1045- 1054.
doi: 10.1186/s12885-021-08766-9 |
| 7 |
El-Taji O , Al-Mitwalli A , Malik F , et al. Secondary neoplasms of the urinary bladder-clinical management and oncological outcomes[J]. Transl Androl Urol, 2021, 10 (6): 2427- 2434.
doi: 10.21037/tau-20-955 |
| 8 |
Beisland C , Talleraas O , Bakke A , et al. Multiple primary malignancies in patients with renal cell carcinoma: A national population-based cohort study[J]. BJU Int, 2006, 97 (4): 698- 702.
doi: 10.1111/j.1464-410X.2006.06004.x |
| 9 |
Koh HM , An HJ , Ko GH , et al. Identification of myoferlin expression for prediction of subsequent primary malignancy in patients with clear cell renal cell carcinoma[J]. In Vivo, 2019, 33 (4): 1103- 1108.
doi: 10.21873/invivo.11579 |
| 10 |
Tian X , Xu WH , Wu JL , et al. Clear cell papillary renal cell carcinoma shares distinct molecular characteristics and may be significantly associated with higher risk of developing second primary malignancy[J]. Pathol Oncol Res, 2021, 27, 1609809.
doi: 10.3389/pore.2021.1609809 |
| 11 |
邱敏, 卢剑, 马潞林, 等. 透明细胞乳头状肾细胞癌的诊治经验[J]. 中华泌尿外科杂志, 2016, 37 (9): 655- 659.
doi: 10.3760/cma.j.issn.1000-6702.2016.09.004 |
| 12 |
Heo J , Noh O K , Oh Y , et al. Second primary cancer after liver transplantation in hepatocellular carcinoma: A nationwide population-based study[J]. Hepatol Int, 2017, 11 (6): 523- 528.
doi: 10.1007/s12072-017-9824-z |
| 13 |
Wang L , Wang H , Wang T , et al. Analysis of polymorphisms in genes associated with the FA/BRCA pathway in three patients with multiple primary malignant neoplasms[J]. Artif Cells Nanomed Biotechnol, 2019, 47 (1): 1101- 1112.
doi: 10.1080/21691401.2019.1575846 |
| 14 | Peng L , Zeng Z , Teng X , et al. Genomic profiling of synchronous triple primary tumors of the lung, thyroid and kidney in a young female patient: A case report[J]. Oncol lett, 2018, 16 (5): 6089- 6094. |
| 15 |
Keegan THM , Bleyer A , Rosenberg AS , et al. Second primary malignant neoplasms and survival in adolescent and young adult cancer survivors[J]. JAMA Oncology, 2017, 3 (11): 1554- 1557.
doi: 10.1001/jamaoncol.2017.0465 |
| 16 |
Cho YY , Lim J , Oh C , et al. Elevated risks of subsequent primary malignancies in patients with thyroid cancer: A nationwide, population-based study in Korea[J]. Cancer, 2015, 121 (2): 259- 268.
doi: 10.1002/cncr.29025 |
| 17 |
Joung JY , Kwon W , Lim J , et al. Second primary cancer risk among kidney cancer patients in Korea: A population-based cohort study[J]. Cancer Res Treat, 2018, 50 (1): 293- 301.
doi: 10.4143/crt.2016.543 |
| 18 | Etiz D , Metcalfe E , Akcay M . Multiple primary malignant neoplasms: A 10-year experience at a single institution from Turkey[J]. J Cancer Res Ther, 2017, 13 (1): 16- 20. |
| [1] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [2] | 刘帅,刘磊,刘茁,张帆,马潞林,田晓军,侯小飞,王国良,赵磊,张树栋. 伴静脉癌栓的肾上腺皮质癌的临床治疗及预后[J]. 北京大学学报(医学版), 2024, 56(4): 624-630. |
| [3] | 虞乐,邓绍晖,张帆,颜野,叶剑飞,张树栋. 具有低度恶性潜能的多房囊性肾肿瘤的临床病理特征及预后[J]. 北京大学学报(医学版), 2024, 56(4): 661-666. |
| [4] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [5] | 方杨毅,李强,黄志高,陆敏,洪锴,张树栋. 睾丸鞘膜高分化乳头状间皮肿瘤1例[J]. 北京大学学报(医学版), 2024, 56(4): 741-744. |
| [6] | 曾媛媛,谢云,陈道南,王瑞兰. 脓毒症患者发生正常甲状腺性病态综合征的相关因素[J]. 北京大学学报(医学版), 2024, 56(3): 526-532. |
| [7] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [8] | 李建斌,吕梦娜,池强,彭一琳,刘鹏程,吴锐. 干燥综合征患者发生重症新型冠状病毒肺炎的早期预测[J]. 北京大学学报(医学版), 2023, 55(6): 1007-1012. |
| [9] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [10] | 薛子璇,唐世英,邱敏,刘承,田晓军,陆敏,董靖晗,马潞林,张树栋. 青年肾肿瘤伴瘤栓的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2023, 55(5): 802-811. |
| [11] | 卢汉,张建运,杨榕,徐乐,李庆祥,郭玉兴,郭传瑸. 下颌牙龈鳞状细胞癌患者预后的影响因素[J]. 北京大学学报(医学版), 2023, 55(4): 702-707. |
| [12] | 时云飞,王豪杰,刘卫平,米岚,龙孟平,刘雁飞,赖玉梅,周立新,刁新婷,李向红. 血管免疫母细胞性T细胞淋巴瘤临床与分子病理学特征分析[J]. 北京大学学报(医学版), 2023, 55(3): 521-529. |
| [13] | 朱晓娟,张虹,张爽,李东,李鑫,徐玲,李挺. 人表皮生长因子受体2低表达乳腺癌的临床病理学特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 243-253. |
| [14] | 赖玉梅,李忠武,李欢,吴艳,时云飞,周立新,楼雨彤,崔传亮. 68例肛管直肠黏膜黑色素瘤临床病理特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 262-269. |
| [15] | 沈棋,刘亿骁,何群. 肾黏液样小管状和梭形细胞癌的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(2): 276-282. |
|
||