北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (4): 729-735. doi: 10.19723/j.issn.1671-167X.2023.04.026
年轻恒牙牙髓再生治疗术后36个月的临床疗效评估
- 北京大学口腔医学院·口腔医院儿童口腔科, 国家口腔医学中心, 国家口腔疾病临床医学研究中心, 口腔生物材料和数字诊疗装备国家工程研究中心, 北京 100081
Retrospective evaluation of treatment outcomes in immature teeth treated with regenerative endodontic procedures with an over-36-month review
Yun-fei DAI,He LIU,Chu-fang PENG,Xi-jun JIANG*( )
)
- Department of Paediatric Dentistry, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing 100081, China
摘要:
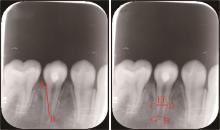
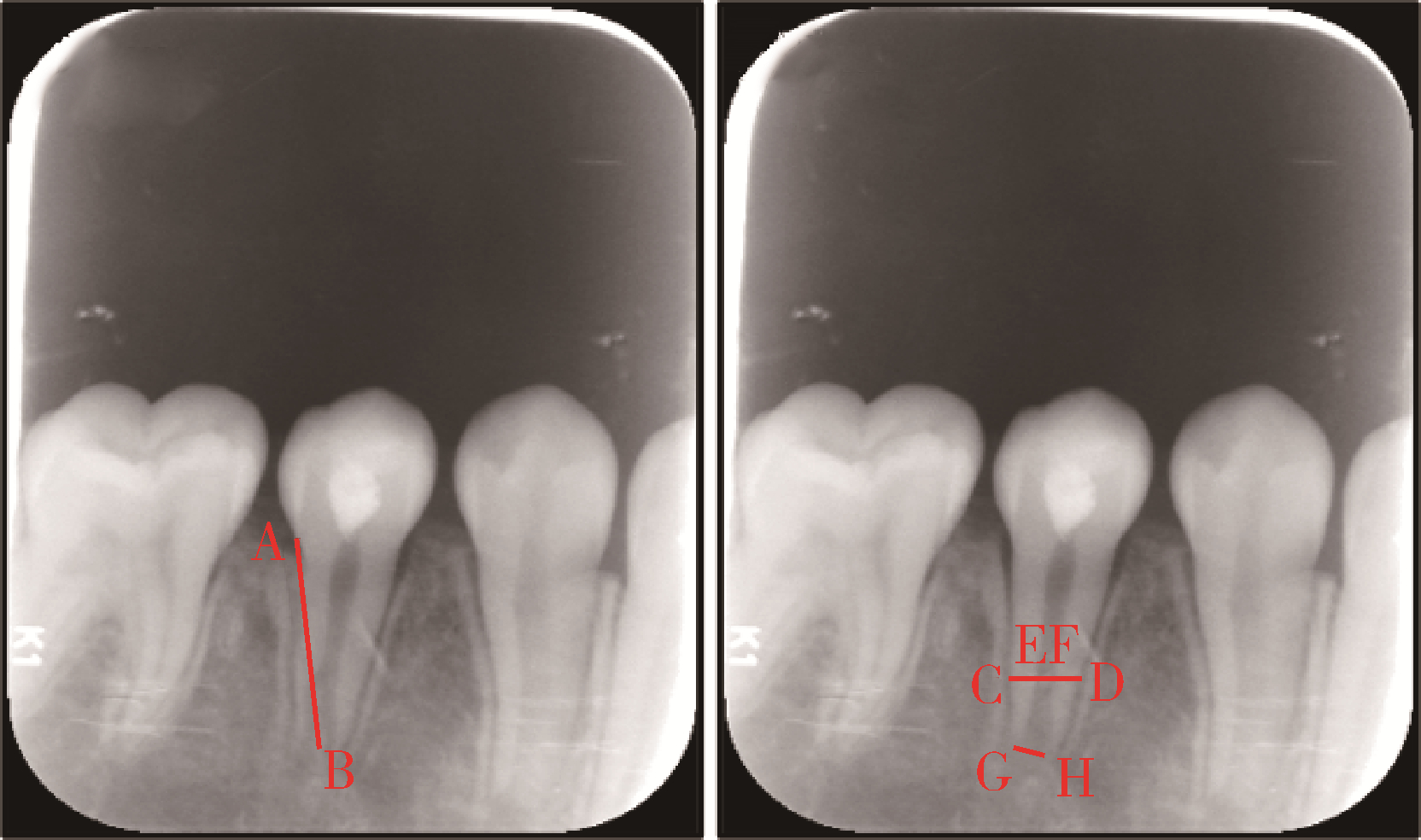
目的: 评价牙髓再生治疗术后36个月以上的临床疗效, 并分析患牙术后牙根继续发育的影响因素, 为长期预后的判断提供依据。方法: 回顾2013年1月至2017年6月在北京大学口腔医院儿童口腔科接受牙髓再生治疗术, 并复查36个月以上的年轻恒牙, 收集治疗前后的临床记录和影像学资料, 评价治疗结果, 总结不同的牙根发育形态。测量并比较治疗前后患牙牙根长度、根管壁厚度和根尖孔直径的变化, 对可能的影响因素进行分析。结果: 共纳入84颗患牙, 最长随访时间81个月, 平均(44.7±19.3)个月。其中68颗(81.0%)患牙临床症状消失, 根尖病变愈合; 55颗(80.9%)患牙的牙根继续发育; 40颗患牙在观察期内根尖孔闭合, 根尖孔闭合率为58.8%;24颗患牙牙根长度、根管壁厚度同时增长且根尖孔闭合, 形态接近生理状态。病因为畸形中央尖折断的患牙的牙根发育率92.5%, 病因为外伤的患牙的牙根发育率为58.3%, 差异有统计学意义(P < 0.05)。术中引血高度不同(根管口/根中部/根尖)的患牙牙根发育率不同(92.9%/81.0%/63.2%), 差异有统计学意义(P < 0.05)。结论: 牙髓再生治疗术后36个月大部分患牙的牙根继续发育, 但是最终牙根形态不同, 部分患牙形态可与正常发育状态相似; 病因和术中引血高度均与牙根能否继续发育显著相关。
中图分类号:
- R788.2
| 1 |
Cehreli ZC , Isbitiren B , Sara S , et al. Regenerative endodontic treatment (revascularization) of immature necrotic molars medicated with calcium hydroxide: A case series[J]. J Endod, 2011, 37 (9): 1327- 1330.
doi: 10.1016/j.joen.2011.05.033 |
| 2 |
Iwaya SI , Ikawa M , Kubota M . Revascularization of an immature permanent tooth with apical periodontitis and sinus tract[J]. Dent Traumatol, 2001, 17 (4): 185- 187.
doi: 10.1034/j.1600-9657.2001.017004185.x |
| 3 |
Almutairi W , Yassen GH , Aminoshariae A , et al. Regenerative endodontics: A systematic analysis of the failed cases[J]. J Endod, 2019, 45 (5): 567- 577.
doi: 10.1016/j.joen.2019.02.004 |
| 4 |
Saoud TM , Zaazou A , Nabil A , et al. Clinical and radiographic outcomes of traumatized immature permanent necrotic teeth after revascularization/revitalization therapy[J]. J Endod, 2014, 40 (12): 1946- 1952.
doi: 10.1016/j.joen.2014.08.023 |
| 5 |
Torabinejad M , Nosrat A , Verma P , et al. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: A systematic review and meta-analysis[J]. J Endod, 2017, 43 (11): 1806- 1820.
doi: 10.1016/j.joen.2017.06.029 |
| 6 |
Shamszadeh S , Asgary S , Nosrat A . Regenerative endodontics: A scientometric and bibliometric analysis[J]. J Endod, 2019, 45 (3): 272- 280.
doi: 10.1016/j.joen.2018.11.010 |
| 7 |
Dohan DM , Choukroun J , Diss A , et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part Ⅰ: Technological concepts and evolution[J]. Oral Surg Oral Med Oral pathol Oral Radiol Endod, 2006, 101 (3): e37- e44.
doi: 10.1016/j.tripleo.2005.07.008 |
| 8 |
Chan EKM , Desmeules M , Cielecki M , et al. Longitudinal cohort study of regenerative endodontic treatment for immature necrotic permanent teeth[J]. J Endod, 2017, 43 (3): 395- 400.
doi: 10.1016/j.joen.2016.10.035 |
| 9 |
Bose R , Nummikoski P , Hargreaves K . A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures[J]. J Endod, 2009, 35 (10): 1343- 1349.
doi: 10.1016/j.joen.2009.06.021 |
| 10 |
Song M , Cao Y , Shin SJ , et al. Revascularization-associated intracanal calcification: Assessment of prevalence and contributing factors[J]. J Endod, 2017, 43 (12): 2025- 2033.
doi: 10.1016/j.joen.2017.06.018 |
| 11 |
Lin J , Zeng Q , Wei X , et al. Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: A prospective randomized controlled study[J]. J Endod, 2017, 43 (11): 1821- 1827.
doi: 10.1016/j.joen.2017.06.023 |
| 12 |
Chen MYH , Chen KL , Chen CA , et al. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures[J]. Int Endod J, 2012, 45 (3): 294- 305.
doi: 10.1111/j.1365-2591.2011.01978.x |
| 13 | Nolla CM . The development of the permanent teeth[J]. J Dent Child, 1960, 27, 254- 266. |
| 14 |
Jung IY , Kim ES , Lee CY , et al. Continued development of the root separated from the main root[J]. J Endod, 2011, 37 (5): 711- 714.
doi: 10.1016/j.joen.2011.01.015 |
| 15 |
Banchs F , Trope M . Revascularization of immature permanent teeth with apical periodontitis: New treatment protocol?[J]. J Endod, 2004, 30 (4): 196- 200.
doi: 10.1097/00004770-200404000-00003 |
| 16 | Civinini R , Macera A , Redl B , et al. The use of autologous blood-derived growth factors in bone regeneration[J]. Clin Cases Miner Bone Metab, 2011, 8 (1): 25- 31. |
| 17 |
Yassen GH , Sabrah AHA , Eckert GJ , et al. Effect of different endodontic regeneration protocols on wettability, roughness, and chemical composition of surface dentin[J]. J Endod, 2015, 41 (6): 956- 960.
doi: 10.1016/j.joen.2015.02.023 |
| 18 |
Shah N , Logani A , Bhaskar U , et al. Efficacy of revascularization to induce apexification/apexogensis in infected, nonvital, immature teeth: A pilot clinical study[J]. J Endod, 2008, 34 (8): 919- 925.
doi: 10.1016/j.joen.2008.05.001 |
| [1] | 郑佳佳,杨雪,温泉,付元,邵校,丁美丽. 生物活性陶瓷iRoot BP Plus®在儿童年轻恒前牙复杂冠折牙髓切断术中的应用[J]. 北京大学学报(医学版), 2024, 56(1): 179-184. |
| [2] | 章锦花,潘洁,孙志鹏,王霄. 不同根管内容物对口腔颌面锥形束CT诊断牙根纵裂准确性的影响[J]. 北京大学学报(医学版), 2023, 55(2): 333-338. |
| [3] | 高娟,吕航苗,马慧敏,赵一姣,李小彤. 锥形束CT三维体积测量评估骨性Ⅲ类错 |
| [4] | 闫文娟,钟洁,林碧琛,丁美丽,陈小贤. 常温流动牙胶应用于根尖诱导成形术后根管充填[J]. 北京大学学报(医学版), 2022, 54(1): 77-82. |
| [5] | 杨雨卉,黄一平,李巍然. 骨皮质切开加速正畸牙齿移动对牙根吸收的影响[J]. 北京大学学报(医学版), 2021, 53(2): 434-437. |
| [6] | 刘建,王宪娥,吕达,乔敏,张立,孟焕新,徐莉,毛铭馨. 广泛型侵袭性牙周炎患者牙根形态异常与相关致病基因的关联[J]. 北京大学学报(医学版), 2021, 53(1): 16-23. |
| [7] | 谢晓艳,贾淑梅,孙志辉,张祖燕. 分辨率设置与锥形束CT检测牙根外吸收的可靠性[J]. 北京大学学报(医学版), 2019, 51(1): 75-79. |
| [8] | 陆瑾慧,钱军,刘鹤,朱俊霞. 富血小板纤维蛋白应用于年轻恒牙牙髓血运重建术的临床研究[J]. 北京大学学报(医学版), 2018, 50(4): 672-679. |
| [9] | 陈晨,章文欣,戚苈源,高学军,梁宇红. 光学相干断层扫描技术诊断牙根裂的实验研究[J]. 北京大学学报(医学版), 2018, 50(3): 547-552. |
| [10] | 贾鹏程,杨刚,胡文杰,赵一姣,刘木清. 根尖片评估单根牙骨内牙根表面积的准确性[J]. 北京大学学报(医学版), 2018, 50(1): 91-97. |
| [11] | 赵一姣,刘怡,孙玉春,王勇. 一种基于曲率连续算法的冠、根三维数据融合方法[J]. 北京大学学报(医学版), 2017, 49(4): 719-723. |
| [12] | 赵一姣,王斯维,刘怡,王勇. 基于影像学牙周膜解剖特征快速提取活体牙三维牙根形态的方法[J]. 北京大学学报(医学版), 2017, 49(1): 54-059. |
| [13] | 沈潇,施捷,徐莉,焦剑,路瑞芳,孟焕新. 伴错牙合畸形的侵袭性牙周炎患者牙周-正畸联合治疗的临床评价[J]. 北京大学学报(医学版), 2017, 49(1): 60-066. |
| [14] | 田洪琰,于鹏,袁重阳,张娓,仇越秀,李德慧,梁新杰,王晓燕. 树脂基覆膜材料对牙根面保护作用的耐久性[J]. 北京大学学报(医学版), 2016, 48(5): 889-893. |
| [15] | 温馥嘉,陈贵,刘怡. 基于锥形束CT的强支抗内收上前牙病例牙根及牙槽骨的形态学分析[J]. 北京大学学报(医学版), 2016, 48(4): 702-708. |
|
||