北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (2): 272-276. doi: 10.19723/j.issn.1671-167X.2025.02.008
术中回收式自体输血对颈动脉体瘤切除术后肿瘤预后的影响
- 北京大学人民医院血管外科, 北京 100044
Effect of intraoperative blood salvage autotransfusion on the prognosis of patients after carotid body tumor resection
Weihao LI, Jing LI, Xuemin ZHANG, Wei LI, Qingle LI, Xiaoming ZHANG*( )
)
- Department of Vascular Surgery, Peking University People's Hospital, Beijing 100044, China
摘要:
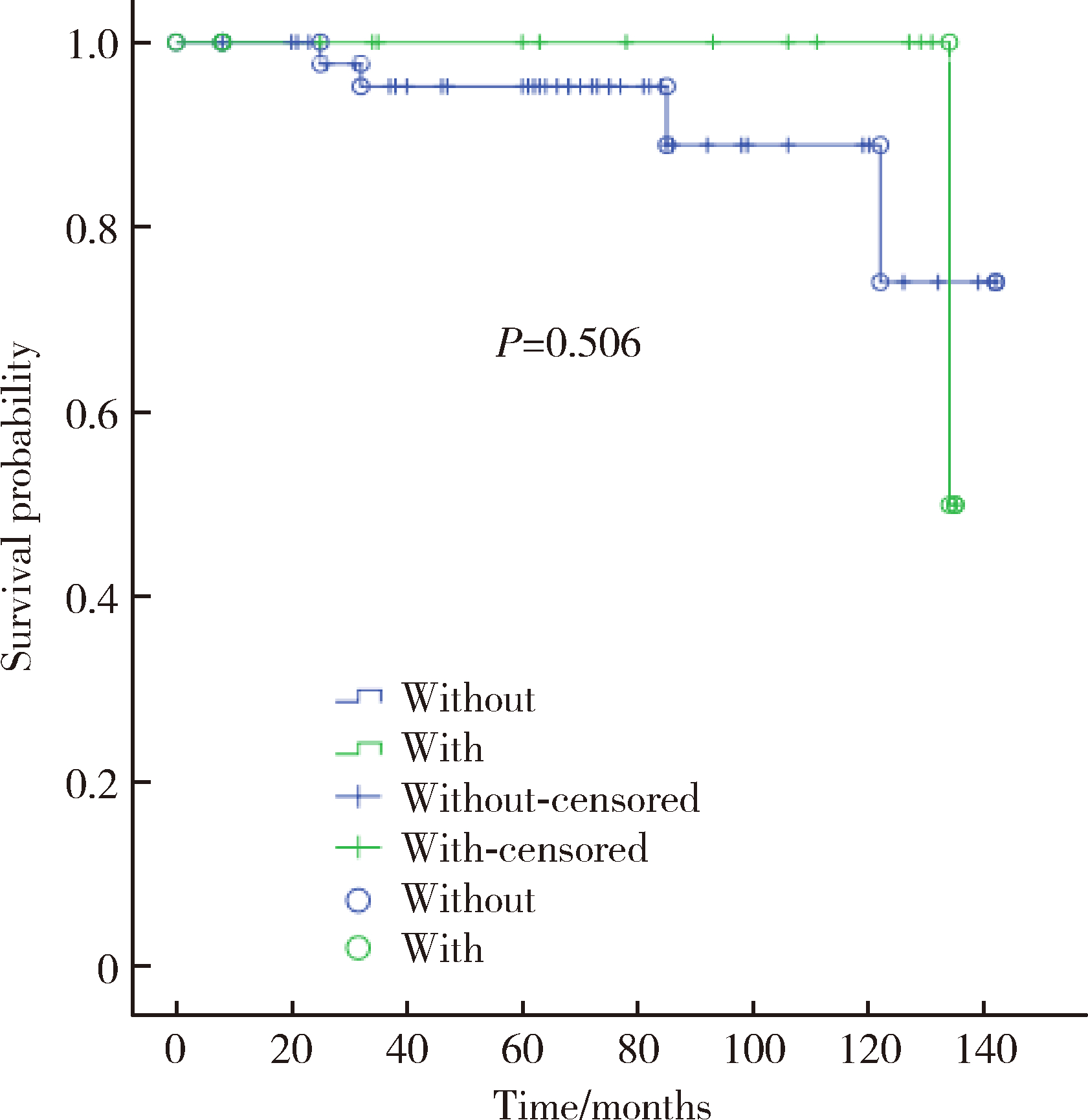
目的: 探讨术中回收式自体输血对颈动脉体瘤切除术后肿瘤局部复发和远期转移的影响。方法: 选择2009年8月至2020年12月在北京大学人民医院血管外科择期行颈动脉体瘤切除术的患者共61例进行回顾性分析, 其中使用术中回收式自体输血者14例, 未使用者47例。收集患者的一般资料、手术情况以及术后随访结果, 分析比较术中自体输血对颈动脉体瘤切除术后患者肿瘤预后的影响。结果: 自体输血组Shamblin Ⅲ型占比85.7%, 显著高于非自体输血组的31.9%(P=0.003)。14例自体输血的患者中, 8例(57%)需同时使用异体血; 而47例非自体输血患者, 6例(13%)需要使用异体血输血, 自体输血组同时使用异体血的比例更高(P =0.002)。术后30 d内神经损伤发生率29.5%, 组间差异无统计学意义。没有发生早期死亡病例。平均随访(76±37)个月, 局部复发1例, 发生于非自体输血组。没有远处转移, 没有肿瘤相关死亡。估计5年总体生存率96.4%, 10年总体生存率83.8%。两组之间总体生存率差异无统计学意义(P =0.506)。结论: 使用术中回收式自体输血不会增加颈动脉体瘤切除术后局部复发和远处转移的风险。
中图分类号:
- R457.1
| 1 |
郭红磊, 贾彦焘. 颈动脉体瘤临床诊疗研究进展[J]. 临床误诊误治, 2021, 34 (3): 108- 112.
doi: 10.3969/j.issn.1002-3429.2021.03.021 |
| 2 |
Moore MG , Netterville JL , Mendenhall WM , et al. Head and neck paragangliomas: An update on evaluation and management[J]. Otolaryngol Head Neck Surg, 2016, 154 (4): 597- 605.
doi: 10.1177/0194599815627667 |
| 3 | 顾光超, 郑月宏. 颈动脉体瘤的影像学检查及外科治疗进展[J]. 血管与腔内血管外科杂志, 2020, 6 (5): 439- 441. |
| 4 |
Butt N , Baek WK , Lachkar S , et al. The carotid body and associated tumors: Updated review with clinical/surgical significance[J]. Br J Neurosurg, 2019, 33 (5): 500- 503.
doi: 10.1080/02688697.2019.1617404 |
| 5 | 马赫, 黄燕娟. 术中回收式自体输血技术适应症的应用[J]. 中南医学科学杂志, 2017, 45 (2): 186- 188. |
| 6 |
李红霞, 韩志强, 钟海燕. 回收式自体输血对肿瘤手术患者预后的影响[J]. 临床输血与检验, 2018, 20 (1): 106- 108.
doi: 10.3969/j.issn.1671-2587.2018.01.036 |
| 7 |
李晶, 蒋京军, 张小明, 等. 颈动脉转流管在复杂颈动脉体瘤手术切除中的应用[J]. 中国普通外科杂志, 2018, 27 (12): 1556- 1562.
doi: 10.7659/j.issn.1005-6947.2018.12.010 |
| 8 | 孔祥国, 李楠, 杨建勇, 等. 术前经导管动脉栓塞对ShamblinⅡ/Ⅲ型颈动脉体瘤切除术的影响[J]. 中山大学学报(医学科学版), 2021, 42 (2): 287- 293. |
| 9 | 吴朋, 吕国士. 64排CT增强扫描结合血管成像对恶性颈动脉体瘤的诊断价值分析[J]. 中国全科医学, 2013, 16 (3): 354- 356. |
| 10 | Mascia D , Esposito G , Ferrante A , et al. Carotid body tumor contemporary management in a high-volume center[J]. J Cardiovasc Surg (Torino), 2020, 61 (4): 459- 466. |
| 11 |
Gu G , Wu X , Ji L , et al. Proposed modification to the Shamblin's classification of carotid body tumors: A single-center retrospective experience of 116 tumors[J]. Eur J Surg Oncol, 2021, 47 (8): 1953- 1960.
doi: 10.1016/j.ejso.2021.03.244 |
| 12 |
Chen Y , Li Y , Liu J , et al. The clinical characteristics and outcomes of carotid body tumors in Chinese patients: A STROBE-compliant observational study[J]. Medicine (Baltimore), 2020, 99 (3): e18824.
doi: 10.1097/MD.0000000000018824 |
| 13 |
Illuminati G , Pasqua R , Nardi P , et al. Results of resection of carotid body tumors with and without lymphnodes' dissection[J]. Surg Oncol, 2021, 37, 101555.
doi: 10.1016/j.suronc.2021.101555 |
| 14 |
王凤明, 章文成, 张仑. 15例恶性颈动脉体瘤的诊断与治疗[J]. 中国肿瘤临床, 2007, 34 (20): 1185- 1187.
doi: 10.3969/j.issn.1000-8179.2007.20.013 |
| 15 |
陶英杰, 刘经祖, 金锐. 10例恶性颈动脉体瘤之生物学行为分析[J]. 中国肿瘤临床, 2001, 28 (4): 288- 289.
doi: 10.3969/j.issn.1000-8179.2001.04.015 |
| 16 | 廖蓉仙, 徐雪梅, 吕豪. 2010—2018年衢州市回收式自体输血发展与思考[J]. 浙江临床医学, 2020, 22 (3): 461- 462. |
| 17 |
汪晓晓, 郭建荣. 自体输血在老年患者手术中的应用价值及风险分析[J]. 临床输血与检验, 2021, 23 (2): 259- 262.
doi: 10.3969/j.issn.1671-2587.2021.02.027 |
| 18 |
Kumar N , Ravikumar N , Tan JYH , et al. Current status of the use of salvaged blood in metastatic spine tumour surgery[J]. Neurospine, 2018, 15 (3): 206- 215.
doi: 10.14245/ns.1836140.070 |
| 19 | 聂晓红, 闫瑞琪, 胡强夫, 等. 术中自体血回输对原发性良性脑膜瘤全切术后肿瘤复发的影响[J]. 广东医学, 2020, 41 (9): 956- 958. |
| 20 |
Bower MR , Ellis SF , Scoggins CR , et al. Phase Ⅱ comparison study of intraoperative autotransfusion for major oncologic procedures[J]. Ann Surg Oncol, 2011, 18 (1): 166- 173.
doi: 10.1245/s10434-010-1228-4 |
| 21 | Elmalky M , Yasin N , Rodrigues-Pinto R , et al. The safety, efficacy, and cost-effectiveness of intraoperative cell salvage in metastatic spine tumor surgery[J]. Spine J, 2017, 17 (7): 977- 982. |
| 22 |
Kinnear N , O'Callaghan M , Hennessey D , et al. Intra-operative cell salvage in urological surgery: A systematic review and meta-analysis of comparative studies[J]. BJU Int, 2019, 123 (2): 210- 219.
doi: 10.1111/bju.14373 |
| 23 |
胡晓云, 陈愉, 赵斌江. 等容血液稀释在颈动脉体瘤手术中的应用[J]. 中国输血杂志, 2000, 13 (4): 251- 252.
doi: 10.3969/j.issn.1004-549X.2000.04.014 |
| 24 | 陈述, 潘静. 稀释法自体输血在颈动脉体瘤手术中的应用(附2例报告)[J]. 齐鲁医学杂志, 2003, 18 (1): 84. |
| [1] | 毛雅晴, 陈震, 于尧, 章文博, 刘洋, 彭歆. 2型糖尿病对口腔鳞状细胞癌患者预后的影响[J]. 北京大学学报(医学版), 2024, 56(6): 1089-1096. |
| [2] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [3] | 刘帅,刘磊,刘茁,张帆,马潞林,田晓军,侯小飞,王国良,赵磊,张树栋. 伴静脉癌栓的肾上腺皮质癌的临床治疗及预后[J]. 北京大学学报(医学版), 2024, 56(4): 624-630. |
| [4] | 虞乐,邓绍晖,张帆,颜野,叶剑飞,张树栋. 具有低度恶性潜能的多房囊性肾肿瘤的临床病理特征及预后[J]. 北京大学学报(医学版), 2024, 56(4): 661-666. |
| [5] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [6] | 方杨毅,李强,黄志高,陆敏,洪锴,张树栋. 睾丸鞘膜高分化乳头状间皮肿瘤1例[J]. 北京大学学报(医学版), 2024, 56(4): 741-744. |
| [7] | 曾媛媛,谢云,陈道南,王瑞兰. 脓毒症患者发生正常甲状腺性病态综合征的相关因素[J]. 北京大学学报(医学版), 2024, 56(3): 526-532. |
| [8] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [9] | 李建斌,吕梦娜,池强,彭一琳,刘鹏程,吴锐. 干燥综合征患者发生重症新型冠状病毒肺炎的早期预测[J]. 北京大学学报(医学版), 2023, 55(6): 1007-1012. |
| [10] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [11] | 薛子璇,唐世英,邱敏,刘承,田晓军,陆敏,董靖晗,马潞林,张树栋. 青年肾肿瘤伴瘤栓的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2023, 55(5): 802-811. |
| [12] | 卢汉,张建运,杨榕,徐乐,李庆祥,郭玉兴,郭传瑸. 下颌牙龈鳞状细胞癌患者预后的影响因素[J]. 北京大学学报(医学版), 2023, 55(4): 702-707. |
| [13] | 时云飞,王豪杰,刘卫平,米岚,龙孟平,刘雁飞,赖玉梅,周立新,刁新婷,李向红. 血管免疫母细胞性T细胞淋巴瘤临床与分子病理学特征分析[J]. 北京大学学报(医学版), 2023, 55(3): 521-529. |
| [14] | 朱晓娟,张虹,张爽,李东,李鑫,徐玲,李挺. 人表皮生长因子受体2低表达乳腺癌的临床病理学特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 243-253. |
| [15] | 赖玉梅,李忠武,李欢,吴艳,时云飞,周立新,楼雨彤,崔传亮. 68例肛管直肠黏膜黑色素瘤临床病理特征及预后[J]. 北京大学学报(医学版), 2023, 55(2): 262-269. |
|
||