北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (4): 644-649. doi: 10.19723/j.issn.1671-167X.2025.04.003
肾透明细胞癌与非透明细胞癌伴静脉癌栓患者的临床病理特征及预后比较
郭博达1,*, 陆敏2,*, 王国良1, 张洪宪1, 刘磊1, 侯小飞1, 赵磊1, 田晓军1, 张树栋1,*( )
)
- 1. 北京大学第三医院泌尿外科, 北京 100191
2. 北京大学基础医学院病理学系, 北京大学第三医院病理科, 北京 100191
Clinicopathological and prognostic differences between clear cell and non-clear cell renal cell carcinoma with venous tumor thrombus
Boda GUO1, Min LU2, Guoliang WANG1, Hongxian ZHANG1, Lei LIU1, Xiaofei HOU1, Lei ZHAO1, Xiaojun TIAN1, Shudong ZHANG1,*( )
)
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Pathology, Peking University Third Hospital, Peking University School of Basic Medical Sciences, Beijing, 100191, China
摘要:
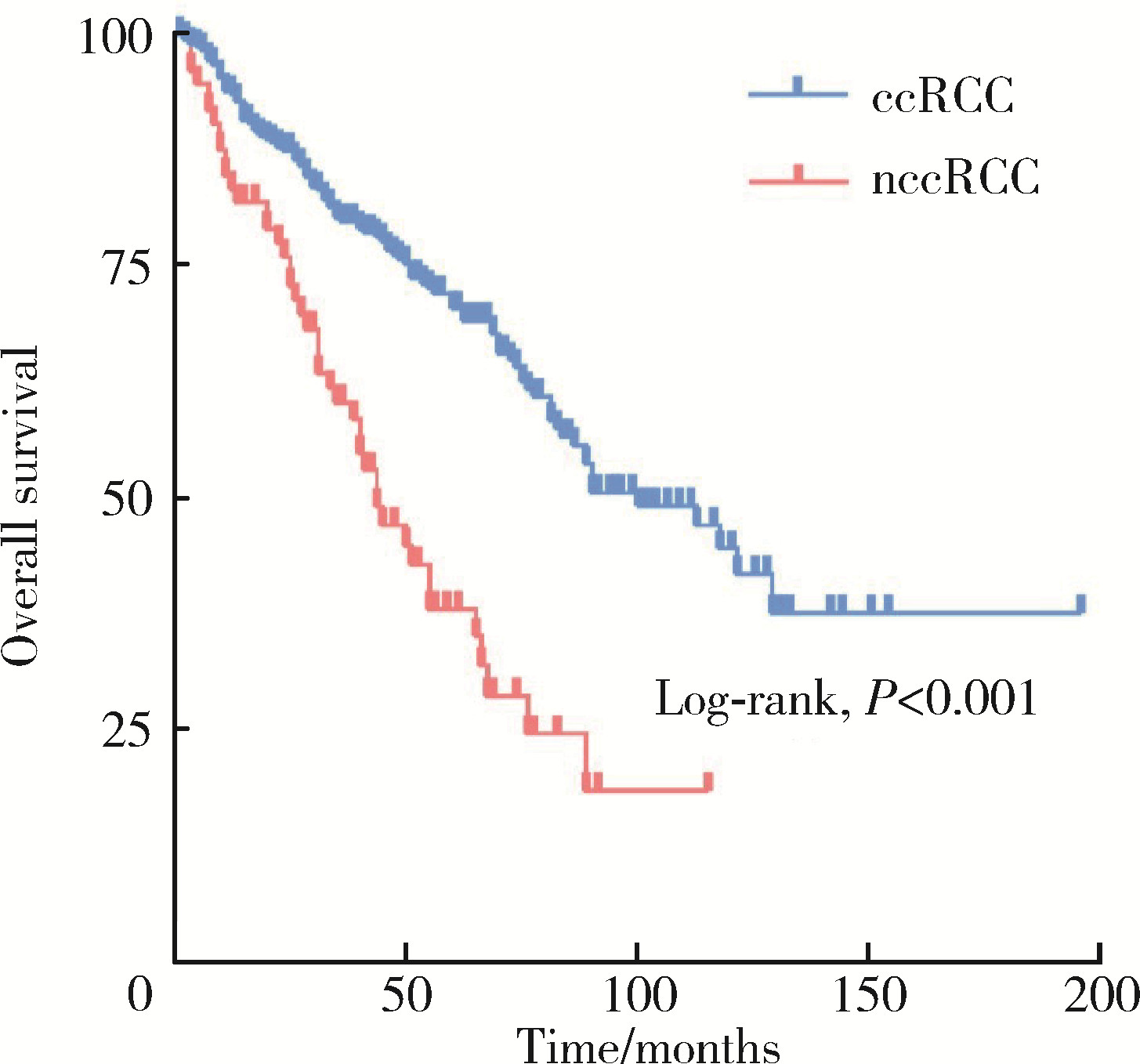
目的: 比较肾透明细胞癌与非透明细胞癌伴静脉癌栓患者的临床病理特征及预后。方法: 连续性纳入2014年1月至2024年2月北京大学第三医院泌尿外科收治的肾细胞癌伴静脉癌栓患者的临床和病理资料进行回顾性分析, 根据病理类型分为透明细胞癌组和非透明细胞癌组, 比较两组患者基线、术中和预后情况。采用Kaplan-Meier方法绘制生存曲线。结果: 共纳入437例患者, 中位年龄58岁, 男性317例, 女性120例, 透明细胞癌组366例, 非透明细胞癌组71例。非透明细胞癌组包括乳头状肾细胞癌38例(53.5%)、嫌色细胞肾细胞癌2例(2.8%)、未分类肾细胞癌11例(15.5%)、分子定义的肾细胞癌19例(26.8%)和肾集合管癌1例(1.4%)。相较于肾透明细胞癌组, 非透明细胞癌组患者发病年龄较早(59岁vs. 55岁, P=0.010), 肿瘤直径更大(8.4 cm vs. 9.5 cm, P=0.025)、淋巴结转移比例较高(56.8% vs. 70.6%, P=0.034)、癌栓分级(P < 0.001)和病理分级较晚(P=0.010)、手术时间较长(272 min vs. 289 min, P=0.023)、总生存期较短(80个月vs. 35个月, P < 0.001)。多因素Cox分析显示与肾细胞癌伴静脉癌栓患者预后相关的因素为病理类型、远处转移、癌栓分级、肉瘤样或横纹肌样分化。两组在性别、体重指数、肿瘤侧别、远处转移、肉瘤样或横纹肌样分化、美国麻醉医师协会评分、手术方式选择、转为开放手术比例、失血量、输注红细胞、输注血浆等方面差异均无统计学意义。结论: 相较于肾透明细胞癌伴静脉癌栓患者, 非透明细胞癌伴静脉癌栓患者发病年龄早、疾病侵袭性强、预后差。
中图分类号:
- R737.11
| 1 |
|
| 2 |
|
| 3 |
|
| 4 |
|
| 5 |
|
| 6 |
|
| 7 |
|
| 8 |
|
| 9 |
|
| 10 |
薛子璇, 唐世英, 邱敏, 等. 青年肾肿瘤伴瘤栓的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2023, 55 (5): 802- 811.
doi: 10.19723/j.issn.1671-167X.2023.05.005 |
| 11 |
|
| 12 |
|
| 13 |
|
| 14 |
|
| 15 |
|
| 16 |
|
| 17 |
|
| [1] | 张展奕, 陆敏, 孙悦皓, 董靖晗, 侯小飞, 肖春雷, 王国良, 田晓军, 马潞林, 张洪宪, 张树栋. TFE3重排肾细胞癌合并静脉癌栓患者的临床病理特征及生存分析[J]. 北京大学学报(医学版), 2025, 57(4): 650-661. |
| [2] | 周泽臻, 葛力源, 张帆, 邓绍晖, 颜野, 张洪宪, 王国良, 刘磊, 黄毅, 张树栋. 病理T3a期肾细胞癌肾部分切除与根治性肾切除的回顾性匹配研究[J]. 北京大学学报(医学版), 2025, 57(4): 704-710. |
| [3] | 李伟浩, 李晶, 张学民, 李伟, 李清乐, 张小明. 术中回收式自体输血对颈动脉体瘤切除术后肿瘤预后的影响[J]. 北京大学学报(医学版), 2025, 57(2): 272-276. |
| [4] | 毛雅晴, 陈震, 于尧, 章文博, 刘洋, 彭歆. 2型糖尿病对口腔鳞状细胞癌患者预后的影响[J]. 北京大学学报(医学版), 2024, 56(6): 1089-1096. |
| [5] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [6] | 刘帅,刘磊,刘茁,张帆,马潞林,田晓军,侯小飞,王国良,赵磊,张树栋. 伴静脉癌栓的肾上腺皮质癌的临床治疗及预后[J]. 北京大学学报(医学版), 2024, 56(4): 624-630. |
| [7] | 虞乐,邓绍晖,张帆,颜野,叶剑飞,张树栋. 具有低度恶性潜能的多房囊性肾肿瘤的临床病理特征及预后[J]. 北京大学学报(医学版), 2024, 56(4): 661-666. |
| [8] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [9] | 方杨毅,李强,黄志高,陆敏,洪锴,张树栋. 睾丸鞘膜高分化乳头状间皮肿瘤1例[J]. 北京大学学报(医学版), 2024, 56(4): 741-744. |
| [10] | 曾媛媛,谢云,陈道南,王瑞兰. 脓毒症患者发生正常甲状腺性病态综合征的相关因素[J]. 北京大学学报(医学版), 2024, 56(3): 526-532. |
| [11] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [12] | 李建斌,吕梦娜,池强,彭一琳,刘鹏程,吴锐. 干燥综合征患者发生重症新型冠状病毒肺炎的早期预测[J]. 北京大学学报(医学版), 2023, 55(6): 1007-1012. |
| [13] | 刘欢锐,彭祥,李森林,苟欣. 基于HER-2相关基因构建风险模型用于膀胱癌生存预后评估[J]. 北京大学学报(医学版), 2023, 55(5): 793-801. |
| [14] | 薛子璇,唐世英,邱敏,刘承,田晓军,陆敏,董靖晗,马潞林,张树栋. 青年肾肿瘤伴瘤栓的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2023, 55(5): 802-811. |
| [15] | 兰东,刘茁,李宇轩,王国良,田晓军,马潞林,张树栋,张洪宪. 根治性肾切除和静脉癌栓取出术大出血的危险因素[J]. 北京大学学报(医学版), 2023, 55(5): 825-832. |
|
||