北京大学学报(医学版) ›› 2021, Vol. 53 ›› Issue (5): 928-932. doi: 10.19723/j.issn.1671-167X.2021.05.019
肾细胞癌合并尿路瘤栓的临床病理特征: 6例报道及文献回顾
- 1.北京大学第三医院泌尿外科,北京 100191
2.首都医科大学附属北京友谊医院放射科,北京 100050
3.北京大学第三医院病理科,北京 100191
Clinical and pathological features of renal cell carcinoma with urinary tract tumor thrombus: 6 cases report and literature review
TIAN Yu1,CHENG Xiao-yue2,HE Hui-ying3,WANG Guo-liang1,△( ),MA Lu-lin1
),MA Lu-lin1
- 1. Department of Urology, Peking University Third Hospital, Beijing 100191, China
2. Department of Radiology, Beijing Friendship Hospital, Capital Medical University, Beijing 100050, China
3. Department of Pathology, Peking University Third Hospital, Beijing 100191, China
摘要:
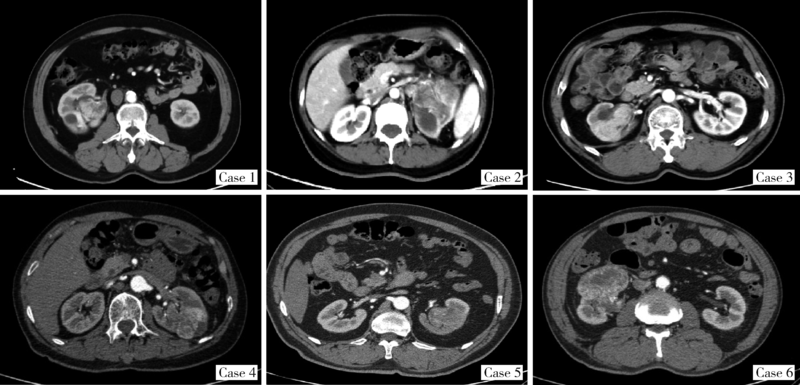
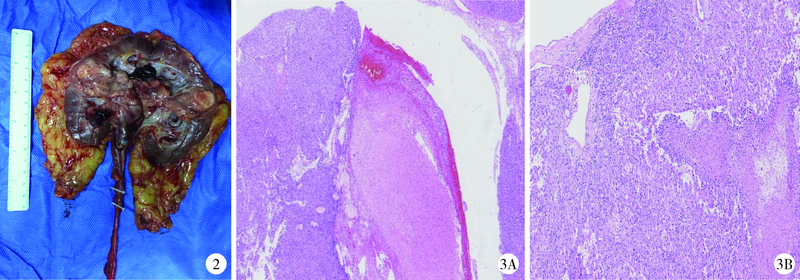
目的: 探讨肾细胞癌合并尿路瘤栓的临床和病理特征。方法: 回顾性分析2015年1月1日至2019年12月31日在北京大学第三医院和首都医科大学附属北京友谊医院住院手术治疗肾细胞癌合并尿路瘤栓患者的基本信息、临床表现、治疗情况、病理特点和随访情况,同时检索文献,将既往报道的此类患者一并列为研究对象。结果: 本研究两家单位共收集到肾细胞癌合并尿路瘤栓患者6例,通过文献检索到16例,共计22例患者,其中男性13例,女性9例,平均年龄54.7岁(22~79岁);左肾15例,右肾6例,病变侧别不明1例;肉眼血尿是最常见的主诉(18例),体质量下降1例,镜下血尿1例,超声检查发现1例,就诊原因不明1例;瘤栓分级为Ⅰ级9例,Ⅱ级10例,Ⅲ级3例;术前诊断肾细胞癌的有11例,术前考虑肾盂癌或不能明确诊断者11例;行肾癌根治性切除术者9例,肾输尿管全长切除术者12例,1例手术方式不明;术后组织病理报告为透明细胞型肾细胞癌15例,乳头状肾细胞癌1例,嫌色细胞癌1例,混合细胞肾细胞癌1例,不能明确分型的肾细胞癌4例;11例患者有随访数据,随访3~31个月,有3例6个月内出现了肺转移。结论: 肾细胞癌合并尿路瘤栓临床上少见,在诊断上需与肾盂癌相鉴别,治疗原则可参照同类型肾细胞癌,对于局部进展期患者,手术完整切除是最佳的治疗方法,患者的肿瘤学预后还有待更长期和更大规模的随访观察。
中图分类号:
- R737.11
| [1] |
Munechika H, Kushihashi T, Gokan T, et al. A renal cell carcinoma extending into the renal pelvis simulating transitional cell carcinoma [J]. Urol Radiol, 1990, 12(1):11-14.
pmid: 2333668 |
| [2] | Chen WC, Lee YH, Huang JK. Renal cell carcinoma with renal pelvic extension simulating transitional cell carcinoma: a case report [J]. Zhonghua Yi Xue Za Zhi, 1996, 58(2):147-150. |
| [3] |
Gulati M, Gore JL, Pantuek AJ, et al. Ureteral tumor thrombus from renal cell carcinoma extending into bladder [J]. Urol Oncol, 2007, 25(5):393-395.
doi: 10.1016/j.urolonc.2007.01.011 |
| [4] |
Fujita O, Wada K, Yamasaki T, et al. Renal cell carcinoma with a tumor thrombus in the ureter: a case report [J]. BMC Urol, 2011, 11(16):1-5.
doi: 10.1186/1471-2490-11-1 |
| [5] |
Kitazono MT, Coakley FV, Naeger DM, et al. CT of unusual renal masses invading the pelvicaliceal system: potential mimics of upper tract transitional cell carcinoma [J]. Clin Imaging, 2011, 35(1):77-80.
doi: 10.1016/j.clinimag.2010.02.012 |
| [6] |
Jeong YB, Kim HJ. Is it transitional cell carcinoma or renal cell carcinoma on computed tomography image? [J]. Urology, 2012, 79(3):e42-e43.
doi: 10.1016/j.urology.2011.11.001 |
| [7] | Kakutani S, Kume H, Hirano Y, et al. Renal cell carcinoma with intraluminal spread of the entire upper urinary tract [J]. Case Rep Med, 2013, 2013:371387. |
| [8] |
Li Y, Ding YU, Chen D. Renal cell carcinoma growing into the renal pelvis and mimicking transitional cell carcinoma: A case report and literature review [J]. Oncol Lett, 2015, 9(4):1869-1872.
doi: 10.3892/ol.2015.2898 |
| [9] | 李嘉临, 纪志刚. 肾嫌色细胞癌侵入肾盂一例分析及文献复习 [J]. 国际外科学杂志, 2016, 43(9):625-627. |
| [10] |
Komatsubara M, Yamazaki M, Fujisaki A, et al. Tumor thrombus of renal cell carcinoma extending into the inferior vena cava, ova-rian vein, and ureter treated with neoadjuvant axitinib [J]. Urology, 2016, 95:e3-e4.
doi: 10.1016/j.urology.2016.05.057 |
| [11] | Parikesit D, Mochtar CA, Tanurahardja B, et al. Thrombus-like tumor of renal cell carcinoma mimicking transitional cell carcinoma of kidney: a case report [J]. Urol Case Rep, 2016, 10:26-29. |
| [12] |
Ishikawa T, Izumi K, Kondo T, et al. A case of renal cell carcinoma growing into the renal pelvis with a fibrin cap in the ureter and bladder [J]. Hinyokika Kiyo, 2018, 64(3):117-122.
doi: 10.14989/ActaUrolJap_64_3_117 pmid: 29684961 |
| [13] |
Jeff J, Alessandro P. Clear cell renal cell carcinoma with a urete-ral thrombus [J]. J Endourol Case Rep, 2018, 4(1):159-162.
doi: 10.1089/cren.2018.0067 pmid: 30426074 |
| [14] |
Bowman M, Reinstatler L, Pettus J, et al. An unusual case of renal cell carcinoma with tumor thrombosis of the proximal ureter [J]. Urol Case Rep, 2019, 23:60-61.
doi: 10.1016/j.eucr.2018.12.009 pmid: 30596019 |
| [15] | Kumar L, Jain S, Kaushal S, et al. A case of type 1 papillary renal cell cancer with pelvic tumor thrombus masquerading as urothelial cancer with review of literature [J]. J Endourol Case Rep, 2019, 5(4):157-160. |
| [16] | Riehie JP. Carcinoma of the renal pelvis and ureter. Diagnosis and management of genitourinary cancer [M]. Philadelphia: Saunders, 1988: 323-336. |
| [17] | National Cancer Institute. SEER Stat Fact Sheets: Kidney and renal pelvis cancer [EB/OL]. (2015-11-29) [2020-18-16]. http://seer.cancer.gov/statfacts/html/kidrp.html . |
| [18] | 李松年. 中华影像医学: 泌尿生殖系统卷 [M]. 北京: 人民卫生出版社, 2002. |
| [19] |
Bata P, Tarnoki DL, Tarnoki AD, et al. Transitional cell and clear cell renal carcinoma: Differentiation of distinct histological types with multiphase CT [J]. Acta Radiol, 2014, 55(9):1112-1119.
doi: 10.1177/0284185113510493 pmid: 24243889 |
| [20] | Amin MB, Edge SB, Greene FL, et al. AJCC cancer staging manual [M]. 8th ed. New York: Springer, 2017. |
| [1] | 周泽臻,邓绍晖,颜野,张帆,郝一昌,葛力源,张洪宪,王国良,张树栋. 非转移性T3a肾细胞癌患者3年肿瘤特异性生存期预测[J]. 北京大学学报(医学版), 2024, 56(4): 673-679. |
| [2] | 沈棋,刘亿骁,何群. 肾黏液样小管状和梭形细胞癌的临床病理特点及预后[J]. 北京大学学报(医学版), 2023, 55(2): 276-282. |
| [3] | 许云屹,苏征征,郑林茂,张孟尼,谭珺娅,杨亚蓝,张梦鑫,徐苗,陈铌,陈雪芹,周桥. 转录通读环状RNA rt-circ-HS促进低氧诱导因子1α表达和肾癌细胞增殖与侵袭[J]. 北京大学学报(医学版), 2023, 55(2): 217-227. |
| [4] | 张铨,宋海峰,马冰磊,张喆楠,周朝晖,李傲林,刘军,梁磊,朱时雨,张骞. 术前预后营养指数可作为预测非转移性肾细胞癌预后的指标[J]. 北京大学学报(医学版), 2023, 55(1): 149-155. |
| [5] | 博尔术,洪鹏,张宇,邓绍晖,葛力源,陆敏,李楠,马潞林,张树栋. 乳头状肾细胞癌的临床病理特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(4): 615-620. |
| [6] | 周鑫,李文智. 肾细胞癌极致保肾时代的冷思考[J]. 北京大学学报(医学版), 2022, 54(4): 595-598. |
| [7] | 韩松辰,黄子雄,刘慧鑫,徐涛. 单侧肾细胞癌根治性切除术后的肾功能代偿[J]. 北京大学学报(医学版), 2021, 53(4): 680-685. |
| [8] | 赵勋,颜野,黄晓娟,董靖晗,刘茁,张洪宪,刘承,马潞林. 癌栓粘连血管壁对非转移性肾细胞癌合并下腔静脉癌栓患者手术及预后的影响[J]. 北京大学学报(医学版), 2021, 53(4): 665-670. |
| [9] | 孙争辉,黄晓娟,董靖晗,刘茁,颜野,刘承,马潞林. 临床T1期肾细胞癌肾窦侵犯的危险因素[J]. 北京大学学报(医学版), 2021, 53(4): 659-664. |
| [10] | 于妍斐,何世明,吴宇财,熊盛炜,沈棋,李妍妍,杨风,何群,李学松. 延胡索酸水合酶缺陷型肾细胞癌的临床病理特征及预后[J]. 北京大学学报(医学版), 2021, 53(4): 640-646. |
| [11] | 张晓鹏,黄子雄,于路平,张晓威,李清,刘士军,徐涛. 小肾细胞癌的临床与病理特征分析[J]. 北京大学学报(医学版), 2019, 51(4): 623-627. |
| [12] | 黄子雄,杜依青,张晓鹏,刘士军,徐涛. 肾细胞癌骨转移的临床与病理分析[J]. 北京大学学报(医学版), 2018, 50(5): 811-815. |
| [13] | 丁振山,邱敏,徐梓程,肖若陶,葛力源,马潞林. 乳头状肾细胞癌合并癌栓患者的临床病理分析[J]. 北京大学学报(医学版), 2018, 50(5): 805-810. |
| [14] | 孙静,宋卫东,闫思源,席志军. 氯喹抑制肾癌细胞活性促进舒尼替尼诱导的细胞凋亡[J]. 北京大学学报(医学版), 2018, 50(5): 778-784. |
|
||