北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (2): 254-261. doi: 10.19723/j.issn.1671-167X.2023.02.008
子宫内膜癌微卫星不稳定性分析: 微小微卫星变换的意义
- 北京大学第一医院病理科, 北京 100034
Analysis of microsatellite instability in endometrial cancer: The significance of minimal microsatellite shift
Li LIANG,Xin LI,Lin NONG,Ying DONG,Ji-xin ZHANG,Dong LI,Ting LI*( )
)
- Department of Pathology, Peking University First Hospital, Beijing 100034, China
摘要:
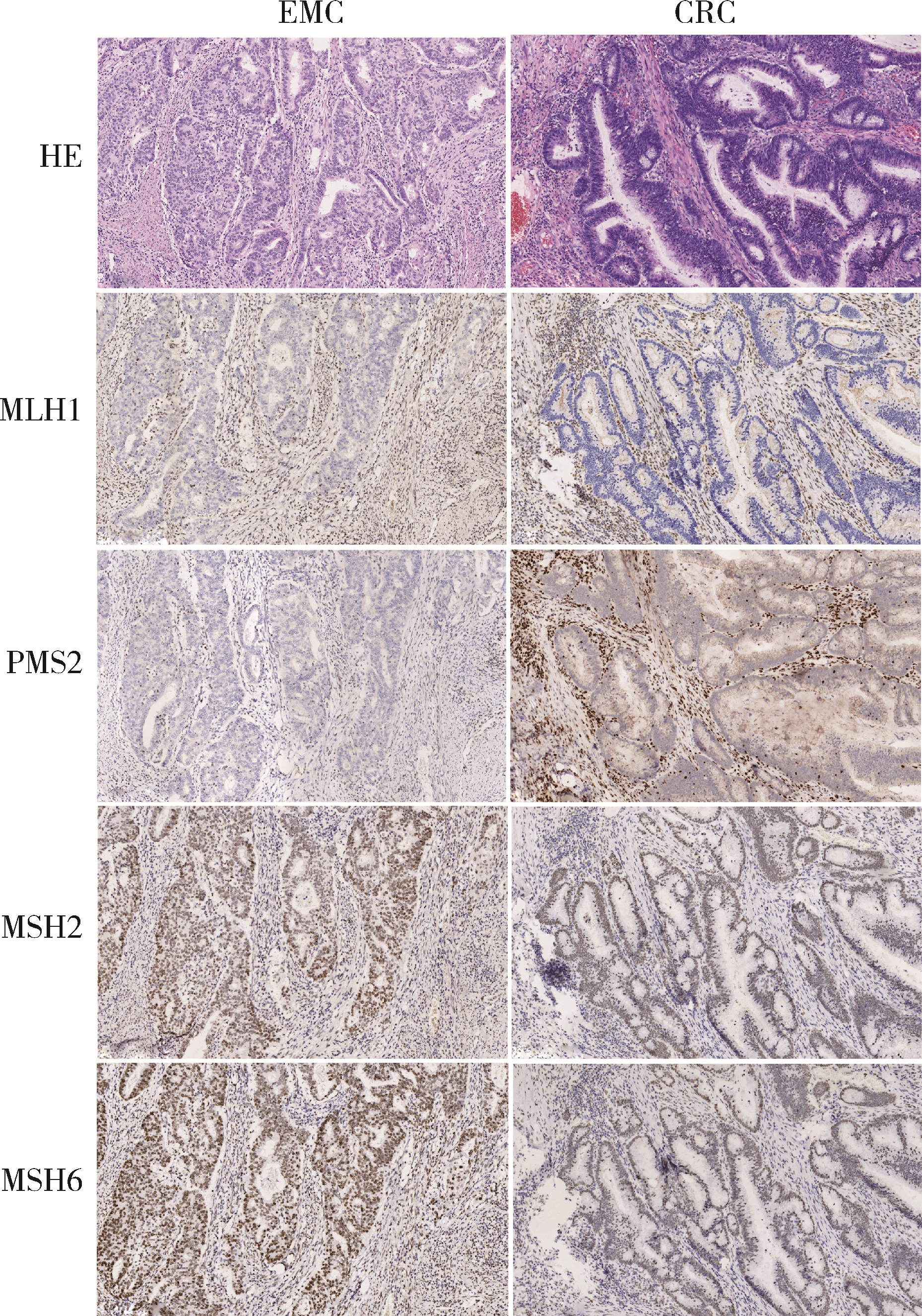
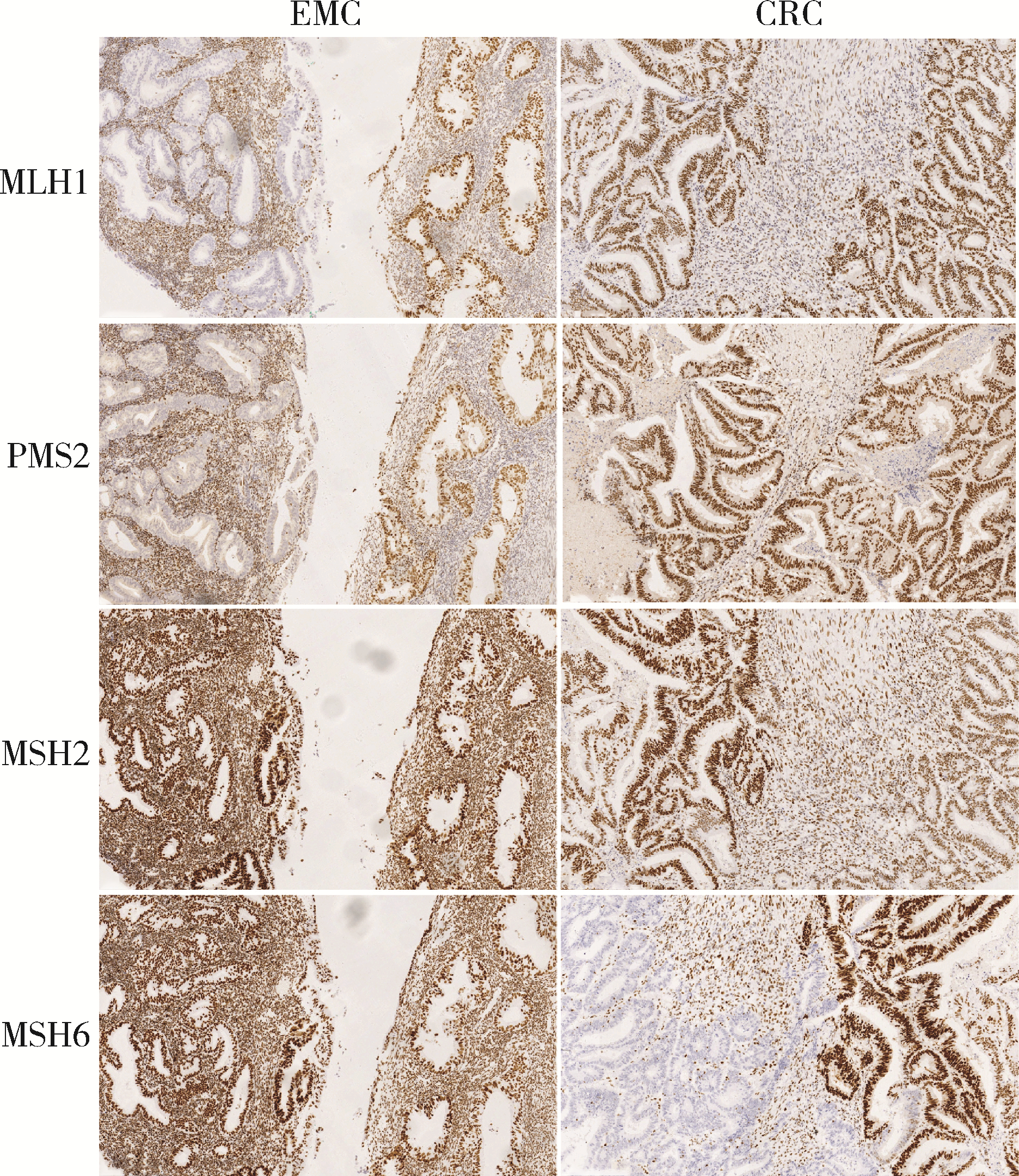
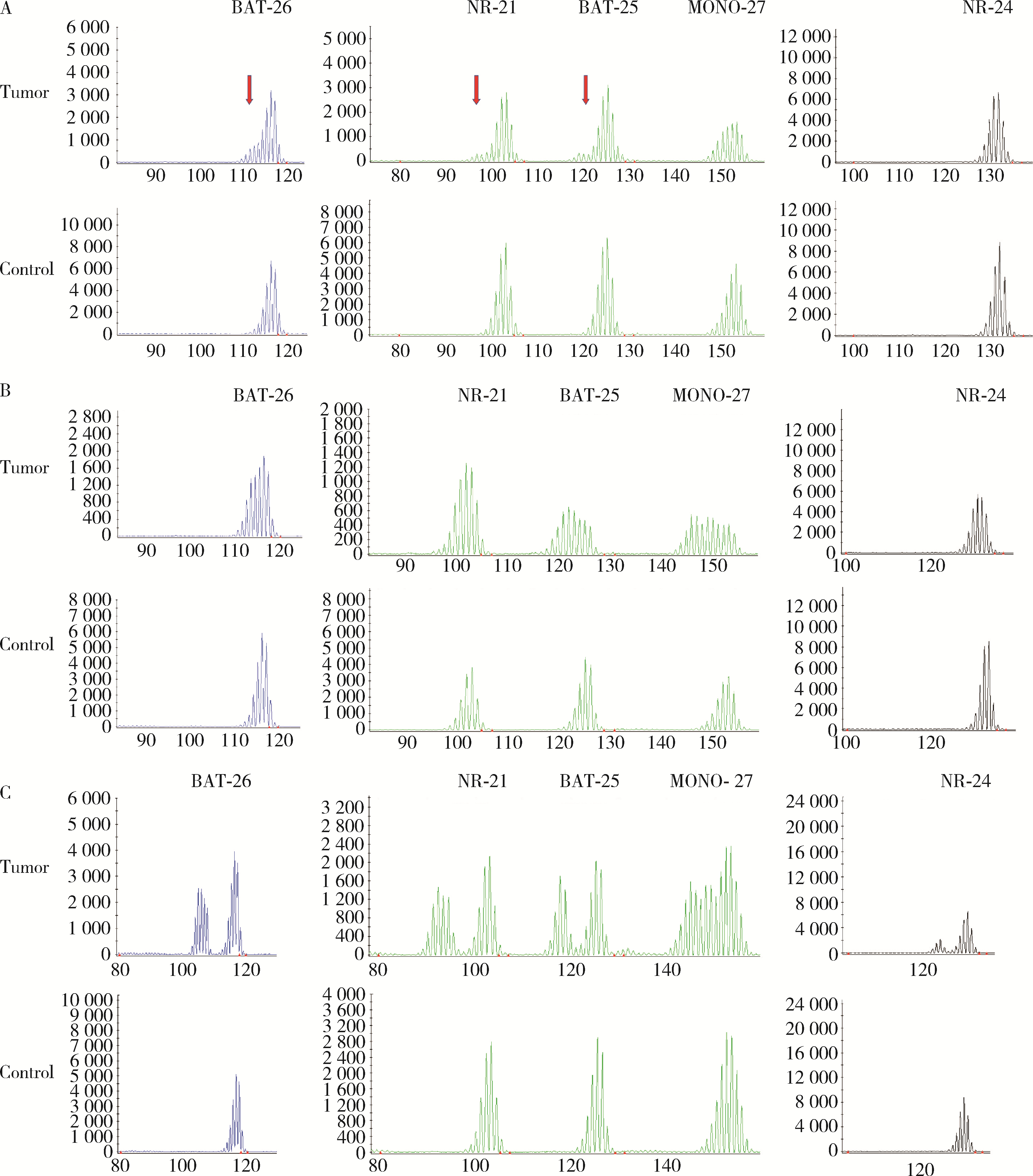
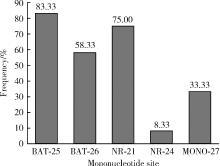
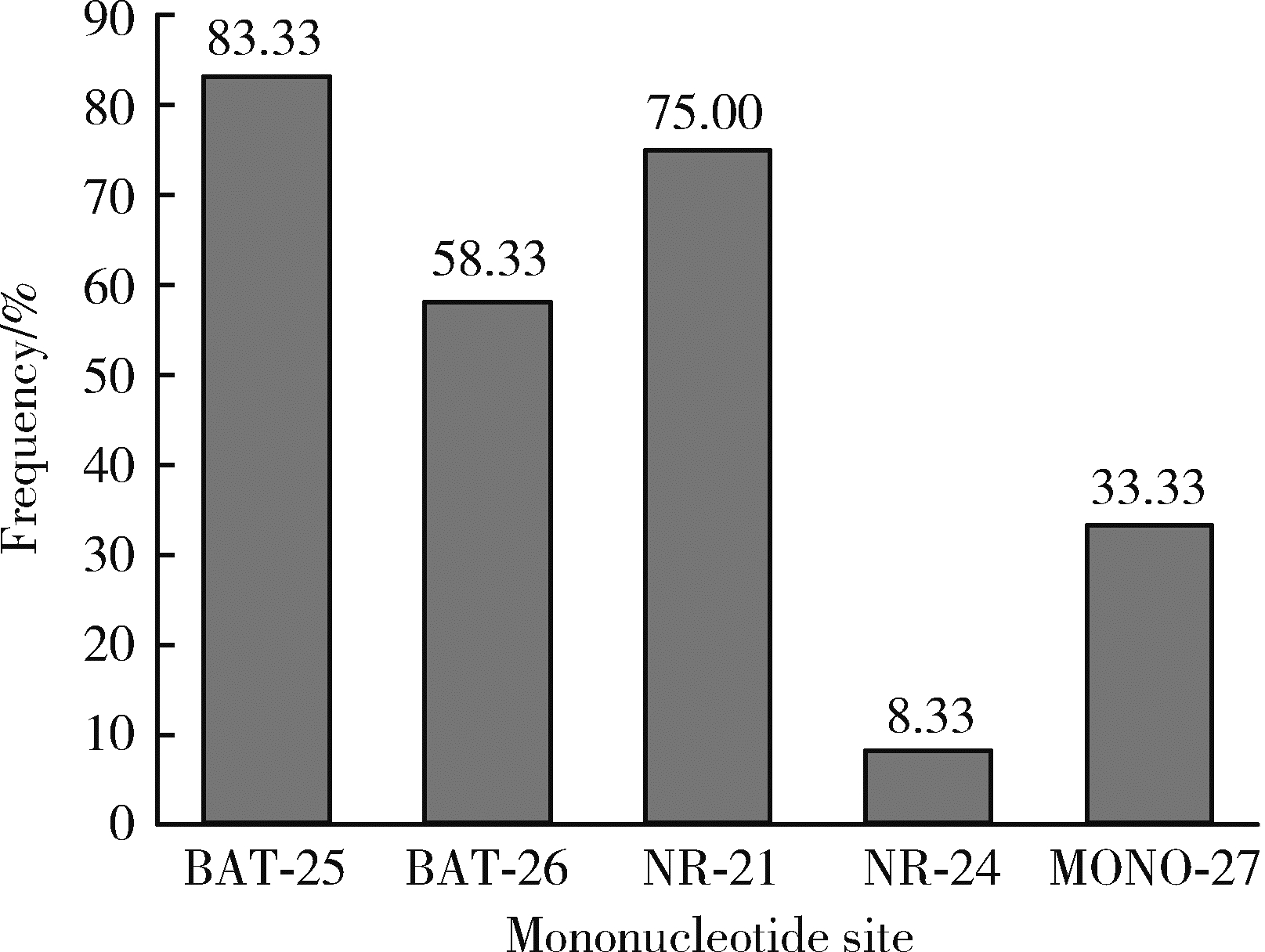
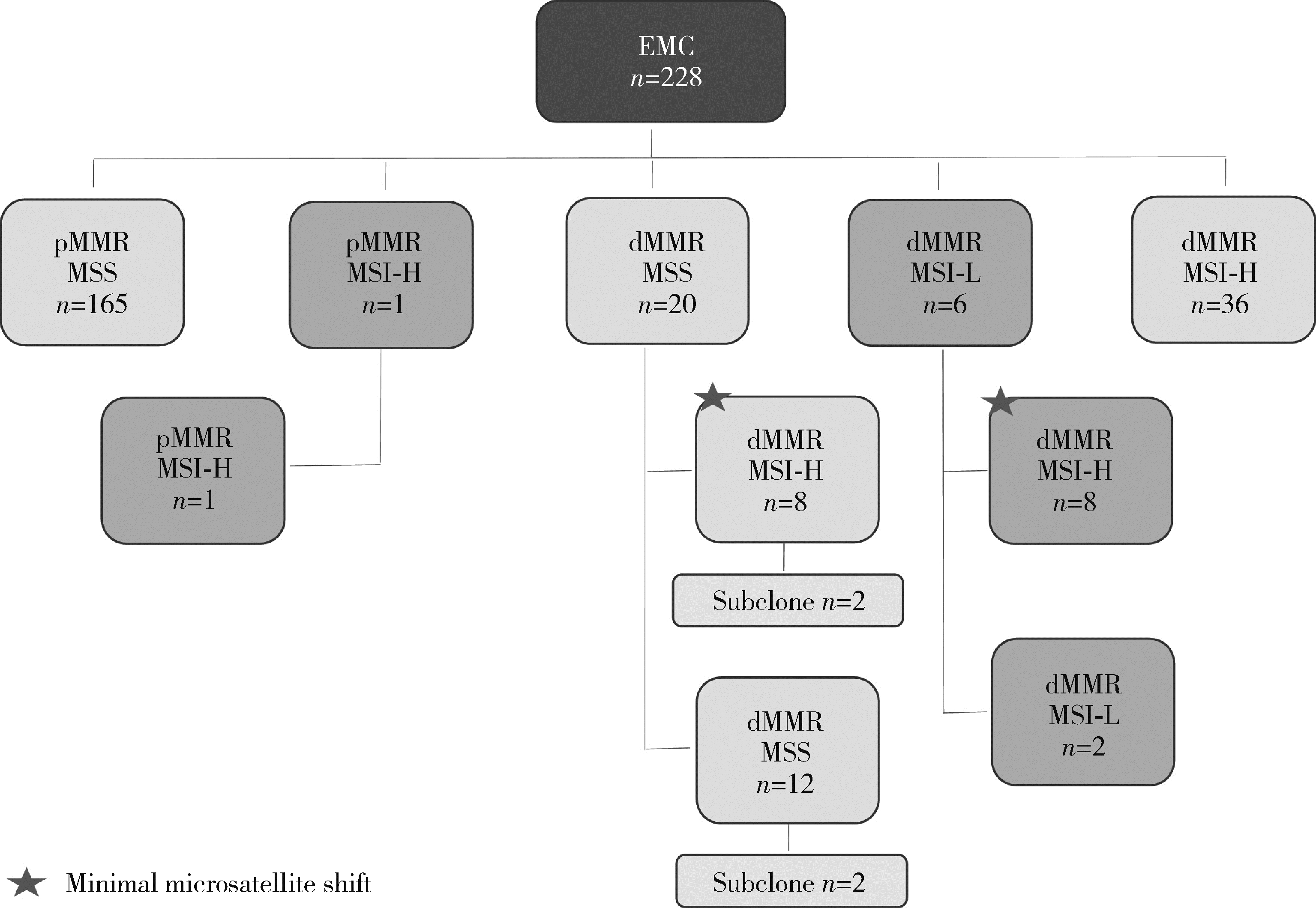
目的: 对比结直肠癌(colorectal cancer, CRC), 评估子宫内膜癌(endometrial cancer, EMC)微卫星不稳定性(microsatellite instability, MSI)改变的特点。方法: 收集228例EMC和770例CRC进行对比分析。采用免疫组织化学(immunohistochemistry, IHC)方法检测错配修复缺陷(deficient mismatch repair, dMMR)蛋白表达缺失, 采用PCR及毛细管电泳片段分析法检测MSI(MSI-PCR), MSI-PCR采用5个单核苷酸位点(BAT-25、BAT-26、NR-21、NR-24和MONO-27)。结果: EMC中, 27.19%(62/228例)为dMMR, 显著高于CRC(7.79%, 60/770例), 且4例dMMR-EMC和2例dMMR-CRC呈错配修复(mismatch repair, MMR)蛋白亚克隆表达。MSI-PCR检测依据显著微卫星变换判读标准, EMC的结果显示: 16.23%(37/228例)为高度MSI, 2.63%(6/228例)为低度MSI, 81.14%(185/228例)为微卫星稳定型, MMR-IHC与MSI-PCR两种评估方法的不一致率为11.84%(27/228例); CRC的结果显示: 8.05%(62/770例)为高度MSI, 0.13%(1/770例)为低度MSI, 91.82%(707/770例)为微卫星稳定型, 两种评估方法的不一致率仅为0.52%(4/770例)。而依据微小微卫星变换结果判读, 12例EMC发现微小微卫星变换(8例dMMR/微卫星稳定型和4例dMMR/低度MSI), 被评估为dMMR/高度MSI, 因此, 高度MSI型EMC为21.49%(49/228例), 两种方法的不一致率降至6.58%(15/228例)。CRC中未见微小微卫星变换。与显著微卫星变换EMC组相比, 微小微卫星变换EMC组的患者年龄偏小, 肿瘤分化更好, 国际妇产科联盟(International Fede-ration of Gyne-cology and Obstetrics, FIGO)分期更早。两组间组织学类型及FIGO分期的差异有统计学意义(P < 0.001, P=0.006)。结论: EMC易发生微小微卫星变换, MSI-PCR检测结果的判读不应忽视微小微卫星变换, MMR-IHC和MSI-PCR互补联合检测是捕获dMMR肿瘤最敏感和特异的方法。
中图分类号:
- R737.33
| 1 |
Yamamoto H , Imai K . Microsatellite instability: An update[J]. Arch Toxicol, 2015, 89 (6): 899- 921.
doi: 10.1007/s00204-015-1474-0 |
| 2 |
Baretti M , Le DT . DNA mismatch repair in cancer[J]. Pharmacol Ther, 2018, 189, 45- 62.
doi: 10.1016/j.pharmthera.2018.04.004 |
| 3 |
Lynch HT , Shaw MW , Magnuson CW , et al. Hereditary factors in cancer. Study of two large midwestern kindreds[J]. Arch Intern Med, 1966, 117 (2): 206- 212.
doi: 10.1001/archinte.1966.03870080050009 |
| 4 |
Dudley JC , Lin MT , Le DT , et al. Microsatellite instability as a biomarker for PD-1 blockade[J]. Clin Cancer Res, 2016, 22 (4): 813- 820.
doi: 10.1158/1078-0432.CCR-15-1678 |
| 5 |
Kandoth C , Schultz N , Cherniack AD , et al. Integrated genomic characterization of endometrial carcinoma[J]. Nature, 2013, 497 (7447): 67- 73.
doi: 10.1038/nature12113 |
| 6 |
Benson AB , Venook AP , Al-Hawary MM , et al. Colon cancer, version 2.2021, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2021, 19 (3): 329- 359.
doi: 10.6004/jnccn.2021.0012 |
| 7 |
Koh WJ , Abu-Rustum NR , Bean S , et al. Uterine neoplasms, version 1.2018, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2018, 16 (2): 170- 199.
doi: 10.6004/jnccn.2018.0006 |
| 8 |
Libera L , Sahnane N , Pepe F , et al. Critical aspects of micro-satellite instability testing in endometrial cancer: A comparison study[J]. Hum Pathol, 2022, 128, 134- 140.
doi: 10.1016/j.humpath.2022.07.014 |
| 9 |
Tafe LJ , Riggs ER , Tsongalis GJ . Lynch syndrome presenting as endometrial cancer[J]. Clin Chem, 2014, 60 (1): 111- 121.
doi: 10.1373/clinchem.2013.206888 |
| 10 |
Recommendations from the EGAPP Working Group . Genetic testing strategies in newly diagnosed individuals with colorectal cancer aimed at reducing morbidity and mortality from Lynch syndrome in relatives[J]. Genet Med, 2009, 11 (1): 35- 41.
doi: 10.1097/GIM.0b013e31818fa2ff |
| 11 |
Wu X , Snir O , Rottmann D , et al. Minimal microsatellite shift in microsatellite instability high endometrial cancer: A significant pitfall in diagnostic interpretation[J]. Mod Pathol, 2019, 32 (5): 650- 658.
doi: 10.1038/s41379-018-0179-3 |
| 12 |
Wang Y , Shi C , Eisenberg R , et al. Differences in microsatellite instability profiles between endometrioid and colorectal cancers: A potential cause for false-negative results?[J]. J Mol Diagn, 2017, 19 (1): 57- 64.
doi: 10.1016/j.jmoldx.2016.07.008 |
| 13 |
Longacre TA , Broaddus R , Chuang LT , et al. Template for reporting results of biomarker testing of specimens from patients with carcinoma of the endometrium[J]. Arch Pathol Lab Med, 2017, 141 (11): 1508- 1512.
doi: 10.5858/arpa.2016-0450-CP |
| 14 |
Cortes-Ciriano I , Lee S , Park WY , et al. A molecular portrait of microsatellite instability across multiple cancers[J]. Nat Commun, 2017, 8, 15180.
doi: 10.1038/ncomms15180 |
| 15 |
Guyot D'Asnières , De Salins A , Tachon G , Cohen R , et al. Discordance between immunochemistry of mismatch repair proteins and molecular testing of microsatellite instability in colorectal cancer[J]. ESMO Open, 2021, 6 (3): 100120.
doi: 10.1016/j.esmoop.2021.100120 |
| 16 |
Ferguson SE , Aronson M , Pollett A , et al. Performance characte-ristics of screening strategies for Lynch syndrome in unselected women with newly diagnosed endometrial cancer who have under-gone universal germline mutation testing[J]. Cancer, 2014, 120 (24): 3932- 3939.
doi: 10.1002/cncr.28933 |
| 17 | McConechy MK , Talhouk A , Li-Chang HH , et al. Detection of DNA mismatch repair (MMR) deficiencies by immunohistoche-mistry can effectively diagnose the microsatellite instability (MSI) phenotype in endometrial carcinomas[J]. Gynecol Oncol, 2014, 137 (2): 306- 310. |
| 18 |
Marshman E , Booth C , Potten CS . The intestinal epithelial stem cell[J]. Bioessays, 2002, 24 (1): 91- 98.
doi: 10.1002/bies.10028 |
| 19 |
Gargett CE , Nguyen HP , Ye L . Endometrial regeneration and endometrial stem/progenitor cells[J]. Rev Endocr Metab Disord, 2012, 13 (4): 235- 251.
doi: 10.1007/s11154-012-9221-9 |
| 20 |
Metcalf AM , Spurdle AB . Endometrial tumour BRAF mutations and MLH1 promoter methylation as predictors of germline mismatch repair gene mutation status: A literature review[J]. Fam Cancer, 2014, 13 (1): 1- 12.
doi: 10.1007/s10689-013-9671-6 |
| 21 | Schweizer P , Moisio AL , Kuismanen SA , et al. Lack of MSH2 and MSH6 characterizes endometrial but not colon carcinomas in hereditary nonpolyposis colorectal cancer[J]. Cancer Res, 2001, 61 (7): 2813- 2815. |
| 22 |
Hampel H , Panescu J , Lockman J , et al. Comment on: Screening for Lynch syndrome (hereditary nonpolyposis colorectal cancer) among endometrial cancer patients[J]. Cancer Res, 2007, 67 (19): 9603.
doi: 10.1158/0008-5472.CAN-07-2308 |
| 23 |
Zhang L . Immunohistochemistry versus microsatellite instability testing for screening colorectal cancer patients at risk for hereditary nonpolyposis colorectal cancer syndrome. Part Ⅱ. The utility of microsatellite instability testing[J]. J Mol Diagn, 2008, 10 (4): 301- 307.
doi: 10.2353/jmoldx.2008.080062 |
| 24 |
Stelloo E , Jansen AML , Osse EM , et al. Practical guidance for mismatch repair-deficiency testing in endometrial cancer[J]. Ann Oncol, 2017, 28 (1): 96- 102.
doi: 10.1093/annonc/mdw542 |
| 25 |
Ta RM , Hecht JL , Lin DI . Discordant loss of mismatch repair proteins in advanced endometrial endometrioid carcinoma compared to paired primary uterine tumors[J]. Gynecol Oncol, 2018, 151 (3): 401- 406.
doi: 10.1016/j.ygyno.2018.10.012 |
| [1] | 森本智惠子,王益勤,周蓉,王建六. 子宫内膜非典型增生及子宫内膜癌患者保留生育功能治疗的临床研究[J]. 北京大学学报(医学版), 2022, 54(5): 936-942. |
| [2] | 丁婷婷,曾楚雄,胡丽娜,余明华. 基于癌症基因组图谱数据库结直肠癌免疫细胞浸润预测模型的建立[J]. 北京大学学报(医学版), 2022, 54(2): 203-208. |
| [3] | 王晓,贺丹,李文婷,阿迪拉·斯依提,韩蕊,董颖. 144例维吾尔族与汉族女性子宫内膜癌微小RNA表达特点及临床意义[J]. 北京大学学报(医学版), 2020, 52(3): 570-577. |
| [4] | 张旭初,张建华,王荣福,范岩,付占立,闫平,赵光宇,白艳霞. 18F-FDG PET/CT联合多种肿瘤标志物在结直肠中分化腺癌术后复发及转移中的应用价值[J]. 北京大学学报(医学版), 2019, 51(6): 1071-1077. |
| [5] | 王小慧,张岩,刘林枝,尚晨光. 二甲双胍与脂联素对子宫内膜癌细胞增殖的作用[J]. 北京大学学报(医学版), 2018, 50(5): 767-773. |
| [6] | 陈杨,王艳荣,石燕,戴广海. 晚期结直肠癌患者一线应用FOLFOX方案化疗引起中性粒细胞减少的预后价值[J]. 北京大学学报(医学版), 2017, 49(4): 669-674. |
| [7] | 刘艳霞,杨雪松,付卫,姚宏伟. 单核苷酸多态性位点rs6983267与溃疡性结肠炎及大肠癌的相关性[J]. 北京大学学报(医学版), 2016, 48(6): 994-999. |
| [8] | 司婧文, 王莉, 巴晓军, 张旭, 董颖, 张继新, 李文婷, 李挺. Lynch综合征临床病理筛查2例及文献回顾[J]. 北京大学学报(医学版), 2015, 47(5): 858-864. |
| [9] | 原春辉,修典荣,葛辉玉,谭石,王行雁,张利,张同琳. 实时虚拟导航系统在结直肠癌肝转移射频消融治疗中的应用[J]. 北京大学学报(医学版), 2013, 45(6): 956-959. |
| [10] | 李传凤, 李军, 白鹏, 吕愈敏. 结直肠腺瘤与患者血脂代谢水平[J]. 北京大学学报(医学版), 2011, 43(3): 432-435. |
| [11] | 汤坚强, 樊庆, 万远廉, 刘玉村, 汪欣, 吴涛, 潘义生, 吴问汉, 朱静. 组织因子/凝血因子Ⅶ在大肠癌中的异位表达及其临床意义[J]. 北京大学学报(医学版), 2009, 41(5): 531-536. |
| [12] | 张耀朋, 吕愈敏, 李军, 韩亚晶, 金珠, 李传凤. 过氧化物酶增殖物激活受体-γ在舒林酸干预治疗大鼠结直肠癌前病变中的作用[J]. 北京大学学报(医学版), 2009, 41(2): 168-173. |
| [13] | 汤坚强, 万远廉, 刘玉村, 戎龙, 汪欣, 吴涛, 潘义生, 朱静. 组织因子/活化凝血Ⅶ因子复合物对大肠癌LoVo细胞系表达基质金属蛋白酶-7的调控作用[J]. 北京大学学报(医学版), 2007, 39(5): 453-457. |
| [14] | 卡马尔, 万远廉, 刘玉村, 汪欣, 崔巍, 王春雷, 陈焕年, 王会元, 朱静. 过氧化物酶增殖物激活受体γ配体曲格列酮对大肠癌细胞生长的影响[J]. 北京大学学报(医学版), 2006, 38(4): 385-388. |
| [15] | 崔巍, 汪欣, 刘玉村, 万远廉, 郭宏杰, 朱静. HIC-5/ARA55在人大肠癌中的表达及其作用机制[J]. 北京大学学报(医学版), 2006, 38(3): 280-283. |
|
||