北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (5): 949-953. doi: 10.19723/j.issn.1671-167X.2019.05.026
角形切口设计和愈合方式与下颌阻生智齿拔除术后并发症
- 北京大学口腔医学院·口腔医院,综合科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
Effect of triangular flap design and healing procedure on the sequelae after extraction of impacted lower third molars
Wei QI,Jian-nan LI,Jing-ren ZHAO,Hai-xia XING,Jie PAN( )
)
- Department of General Dentistry, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing, 100081, China
摘要:
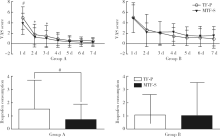
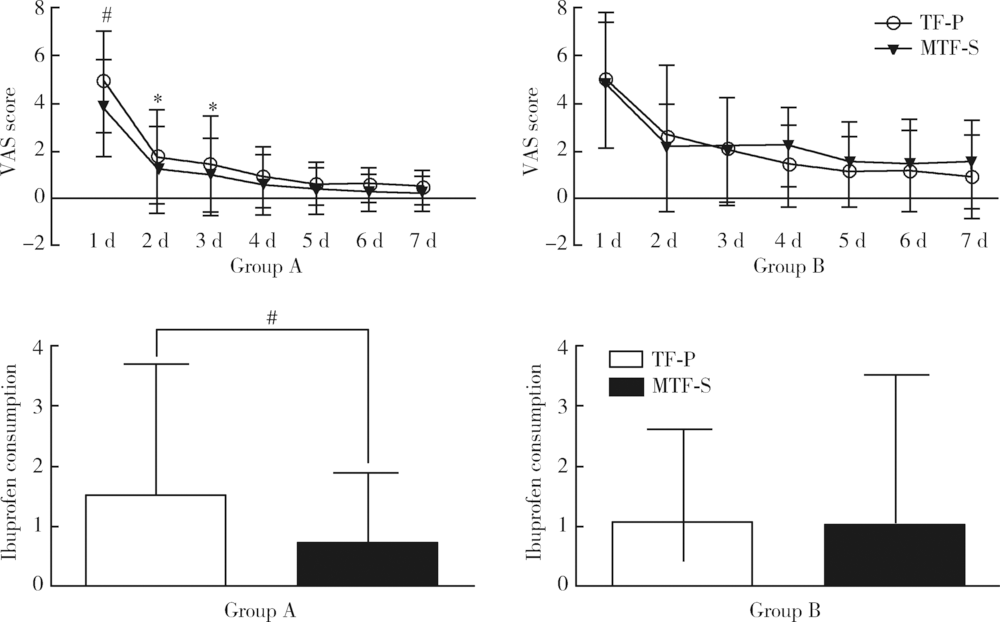
目的:探讨两种角形切口设计和愈合方式对下颌阻生智齿拔除术后并发症的影响。方法:采用分口设计,共纳入60例患者(120侧)。所有患者均有双侧埋伏阻生下颌智齿,且双侧阻生方式相同。按照牙冠是否完全骨埋伏将患者分为A组(冠完全骨埋伏,30例)和B组(冠部分骨埋伏,30例)。一侧采用角形瓣,术后一期缝合完全关闭创口(triangular flap-primary healing,TF-P);对侧采用改良角形瓣,缝合后在第二磨牙远中遗留三角形的牙龈缺损,二期愈合(modified triangular flap-secondary healing,MTF-S)。所有手术由同一医师完成。术后第1天、第3天和第7天复查,检测术后疼痛(VAS评分和布洛芬用量)、肿胀和张口受限程度。术后6个月复查,检查第二磨牙远中探诊深度(probing depth,PD)。配对t检验对比两种方案在术后疼痛、肿胀和开口受限方面的差异。结果:A组中,术后第1天和第3天,MTF-S方案疼痛、肿胀程度低于TF-P方案(P<0.05);术后第1天、第3天和第7天MTF-S方案张口受限程度低于TF-P方案(P<0.05)。B组中,两种方案在术后疼痛、肿胀和张口受限方面差异无统计学意义,但术后第4天,MTF-S方案侧疼痛有加重趋势。术后6个月第二磨牙远中探诊,A、B两组中两种方案的PD差异无统计学意义。结论:MTF-S方案能够减轻完全骨埋伏下颌智齿拔除术后的并发症;术后6个月,两种方案在第二磨牙远中PD方面差异无统计学意义。
中图分类号:
- R782.11
| [1] | Farish SE, Bouloux GF . General technique of third molar removal[J]. Oral Maxillofac Surg Clin North Am, 2007,19(1):23-43. |
| [2] | Cetinkaya BO, Sumer M, Tutkun F , et al. Influence of different suturing techniques on periodontal health of the adjacent second molars after extraction of impacted mandibular third molars[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009,108(2):156-161. |
| [3] | Sanchis Bielsa JM, Hernández-Bazán S, Peáarrocha Diago M . Flap repositioning versus conventional suturing in third molar surgery[J]. Med Oral Patol Oral Cir Bucal, 2008,13(2):E138-142. |
| [4] | Baqain ZH, Al-Shafii A, Hamdan AA , et al. Flap design and mandibular third molar surgery: a split mouth randomized clinical study[J]. Int J Oral Maxillofac Surg, 2012,41(8):1020-1024. |
| [5] | Barone A, Marconcini S, Giacomelli L , et al. A randomized clinical evaluation of ultrasound bone surgery versus traditional rotary instruments in lower third molar extraction[J]. J Oral Maxillofac Surg, 2010,68(2):330-336. |
| [6] | Pasqualini D, Cocero N, Castella A , et al. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: a comparative study[J]. Int J Oral Maxillofac Surg, 2005,34(1):52-57. |
| [7] | Erdogan O, Tatlı U, Ustün Y , et al. Influence of two different flap designs on the sequelae of mandibular third molar surgery[J]. Oral Maxillofac Surg, 2011,15(3):147-152. |
| [8] | Bello SA, Olaitan AA, Ladeinde AL . A randomized comparison of the effect of partial and total wound closure techniques on postoperative morbidity after mandibular third molar surgery[J]. J Oral Maxillofac Surg, 2011,69(6):e24-30. |
| [9] | Cerqueira PR, Vasconcelos BC, Bessa-Nogueira RV . Comparative study of the effect of a tube drain in impacted lower third molar surgery[J]. J Oral Maxillofac Surg, 2004,62(1):57-61. |
| [10] | Jakse N, Bankaoglu V, Wimmer G , et al. Primary wound healing after lower third molar surgery: evaluation of 2 different flap designs[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2002,93(1):7-12. |
| [11] | Kugelberg CF, Ahlström U, Ericson S , et al. Periodontal healing after impacted lower third molar surgery in adolescents and adults. A prospective study[J]. Int J Oral Maxillofac Surg, 1991,20(1):18-24. |
| [12] | Sandhu A, Sandhu S, Kaur T . Comparison of two different flap designs in the surgical removal of bilateral impacted mandibular third molars[J]. Int J Oral Maxillofac Surg, 2010,39(11):1091-1096. |
| [13] | Haraji A, Motamedi MH, Rezvani F . Can flap design influence the incidence of alveolar osteitis following removal of impacted mandibular third molars[J]. Gen Dent, 2010,58(5):e187-189. |
| [14] | Kirk DG, Liston PN, Tong DC , et al. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2007,104(1):e1-6. |
| [15] | Briguglio F, Zenobio EG, Isola G , et al. Complications in surgical removal of impacted mandibular third molars in relation to flap design: clinical and statistical evaluations[J]. Quintessence Int, 2011,42(6):445-453. |
| [16] | Dodson TB . Is there a role for reconstructive techniques to prevent periodontal defects after third molar surgery[J]. Oral Maxillofac Surg Clin North Am, 2007,19(1):99-104. |
| [17] | Peñarrocha Diago M, Galán Gil S, Peáarrocha Diago M . Vestibular bone window for the extraction of impacted lower third molars: four case reports[J]. Med Oral Patol Oral Cir Bucal, 2008,13(8):E508-510. |
| [18] | Dodson TB . Management of mandibular third molar extraction sites to prevent periodontal defects[J]. J Oral Maxillofac Surg, 2004,62(10):1213-1224. |
| [19] | Leung WK, Corbet EF, Kan KW , et al. A regimen of systematic periodontal care after removal of impacted mandibular third molars manages periodontal pockets associated with the mandibular second molars[J]. J Clin Periodontol, 2005,32(7):725-731. |
| [20] | Chen YW, Lee CT, Hum L , et al. Effect of flap design on periodontal healing after impacted third molar extraction: a systematic review and meta-analysis[J]. Int J Oral Maxillofac Surg, 2017,46(3):363-372. |
| [21] | Rosa AL, Carneiro MG, Lavrador MA , et al. Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molars[J]. Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2002,93(4):404-407. |
| [1] | 许素环,王蓓蓓,庞秋颖,钟丽君,丁炎明,黄燕波,车新艳. 等体温膀胱冲洗对经尿道前列腺电切术患者干预效果的meta分析[J]. 北京大学学报(医学版), 2023, 55(4): 676-683. |
| [2] | 李辉,高阳旭,王书磊,姚红新. 恶性肿瘤患儿完全植入式静脉输液港手术并发症[J]. 北京大学学报(医学版), 2022, 54(6): 1167-1171. |
| [3] | 李伟浩,李伟,张学民,李清乐,焦洋,张韬,蒋京军,张小明. 去分支杂交手术和传统手术治疗胸腹主动脉瘤的结果比较[J]. 北京大学学报(医学版), 2022, 54(1): 177-181. |
| [4] | 耿志宇,高为华,王东信. 全身麻醉气管插管患者术后声带运动不良的临床结局[J]. 北京大学学报(医学版), 2021, 53(2): 337-340. |
| [5] | 董文敏,王明瑞,胡浩,王起,许克新,徐涛. Allium覆膜金属输尿管支架长期留置治疗输尿管-回肠吻合口狭窄的初期临床经验及随访结果[J]. 北京大学学报(医学版), 2020, 52(4): 637-641. |
| [6] | 高健,胡立宝,陈尘,郅新,徐涛. 经皮肾镜去石术后出血的介入治疗[J]. 北京大学学报(医学版), 2020, 52(4): 667-671. |
| [7] | 马凯,曲星珂,许清泉,熊六林,叶雄俊,安立哲,陈伟男,黄晓波. 肾移植术后移植肾输尿管膀胱吻合口狭窄的腔内治疗:13例报道[J]. 北京大学学报(医学版), 2019, 51(6): 1155-1158. |
| [8] | 梁晨,张维宇,胡浩,王起,方志伟,许克新. 膀胱扩大术两种不同术式的疗效及并发症比较[J]. 北京大学学报(医学版), 2019, 51(2): 293-297. |
| [9] | 徐稼轩,王宏志,董军,陈小杰,杨勇,陈仁雄,王国栋. 食管癌术后急性肺损伤/急性呼吸窘迫综合征的危险因素分析[J]. 北京大学学报(医学版), 2018, 50(6): 1057-1062. |
| [10] | 李旭, 李奉龙, 鲁谊, 朱以明, 郭斯翊, 李屹钧, 姜春岩. 锁定钢板治疗非骨质疏松性复杂肱骨近端骨折的中期临床及影像学随访研究[J]. 北京大学学报(医学版), 2017, 49(5): 855-860. |
| [11] | 黄珺君,张红,章巍,王玺,龚玉红,王广发. 支气管镜下介入治疗早期并发症的独立危险因素[J]. 北京大学学报(医学版), 2016, 48(6): 1006-1011. |
| [12] | 葛娜,关明,李茜,李率,王恩博. 可弯曲喉罩在颌面外科日间手术的应用[J]. 北京大学学报(医学版), 2015, 47(6): 1010-1014. |
| [13] | 刘坤,徐宗源,孟峻嵩,傅广波,顾硕,顾民. 术前营养风险对根治性全膀胱切除术后并发症发生率的影响[J]. 北京大学学报(医学版), 2015, 47(5): 800-803. |
| [14] | 邵旭, 于炎冰, 张黎, 徐晓利, 许骏, 刘江, 刘红举, 杨文强. 腰骶段选择性脊神经后根切断术治疗脑瘫性下肢痉挛状态手术并发症[J]. 北京大学学报(医学版), 2015, 47(1): 160-164. |
| [15] | 栾景源, 李选, 向勇, 傅军, 王昌明, 李天润, 韩金涛. 腹主动脉瘤腔内修复术中封闭髂内动脉后的并发症[J]. 北京大学学报(医学版), 2014, 46(6): 917-919. |
|
||