北京大学学报(医学版) ›› 2026, Vol. 58 ›› Issue (1): 30-36. doi: 10.19723/j.issn.1671-167X.2026.01.004
口服抗生素辅助牙周机械治疗对重度牙周炎的短期疗效及影响因素
潘莲菲1, 李文静2, 王瑞洋3, 焦剑3, 曹战强4, 高丽1,*( ), 释栋1,*(
), 释栋1,*( )
)
- 1. 北京大学口腔医学院·口腔医院牙周科, 国家口腔医学中心, 国家口腔疾病临床医学研究中心, 口腔生物材料和数字诊疗装备国家工程研究中心, 北京 100081
2. 清华大学北京清华长庚医院口腔医学中心, 北京 102218
3. 北京大学口腔医学院·口腔医院第一门诊部, 北京 100081
4. 北京大学口腔医学院·口腔医院信息中心, 北京 100081
Short-term efficacy and influencing factors of systemic antibiotics as an adjunct to mechanical periodontal therapy for stages Ⅲ/Ⅳ periodontitis
Lianfei PAN1, Wenjing LI2, Ruiyang WANG3, Jian JIAO3, Zhanqiang CAO4, Li GAO1,*( ), Dong SHI1,*(
), Dong SHI1,*( )
)
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing 100081, China
2. Department of Stomatology, Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua Medicine, Tsinghua University, Beijing 102218, China
3. First Clinical Division, Peking University School and Hospital of Stomatology, Beijing 100081, China
4. Information Center, Peking University School and Hospital of Stomatology, Beijing 100081, China
摘要:
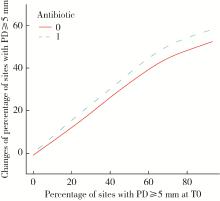
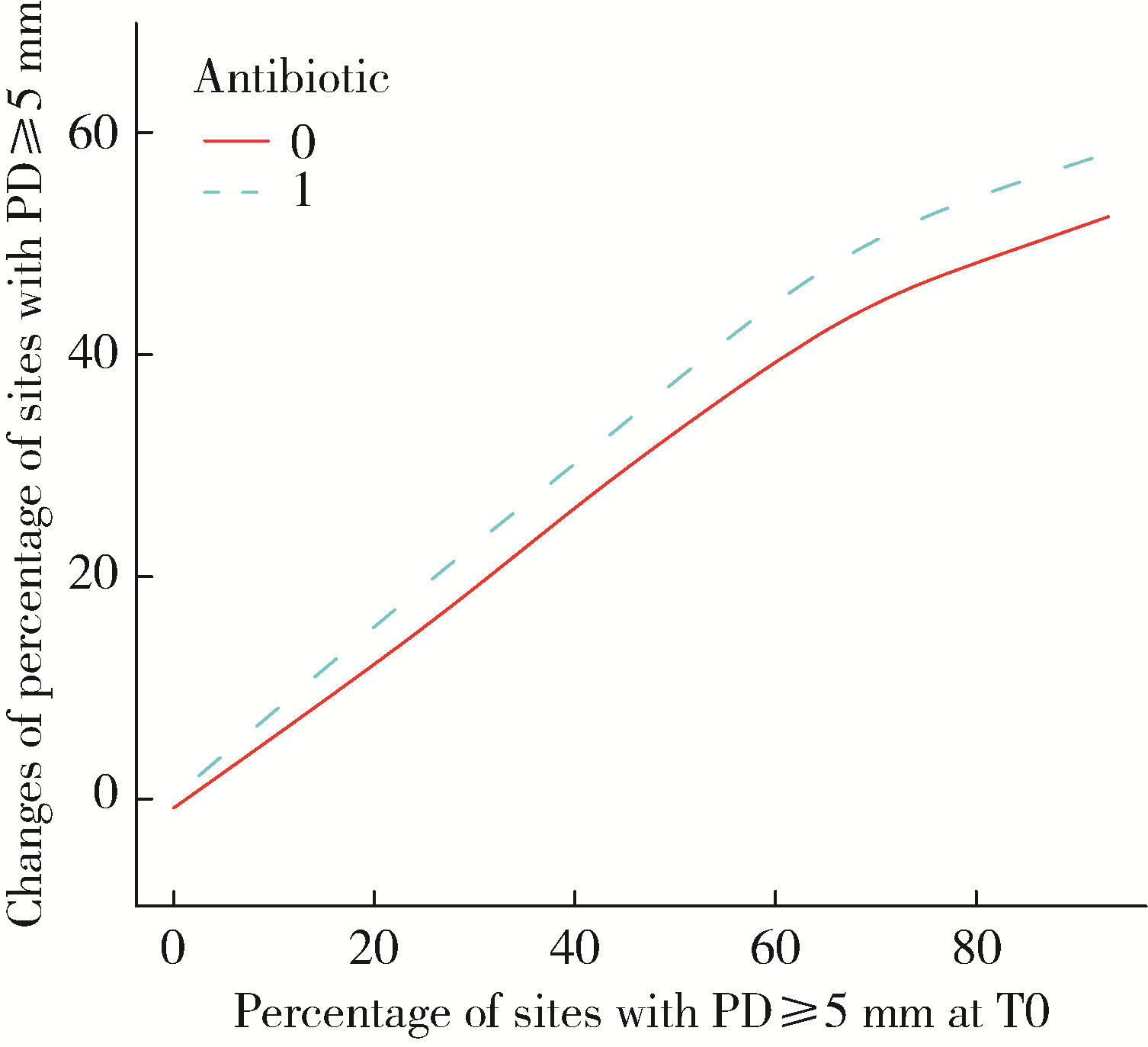
目的: 评价全身应用抗生素对Ⅲ期和Ⅳ期牙周炎患者牙周机械治疗短期疗效的辅助作用, 并探索影响疗效的关键因素, 为临床精准用药提供参考。方法: 选择2007年11月至2015年2月在北京大学口腔医院牙周科接受过牙周机械治疗的患者的病例资料进行回顾性分析, 共纳入521例Ⅲ/Ⅳ期牙周炎患者, 根据是否在龈下刮治和根面平整(scaling and root planing, SRP)基础上全身应用抗生素, 将患者分为抗生素组(n=204)和非抗生素组(n=317), 根据抗生素使用时机将抗生素组分为SRP前, SRP中和SRP后3个亚组。主要结局指标为探诊深度(probing depth, PD)≥5 mm的位点百分比变化。通过单因素线性回归分析确定各因素与疗效的关联, 采用多因素线性回归分析确定抗生素使用、抗生素组年龄和用药时机等因素与疗效的关联, 进一步采用平滑曲线拟合与分段线性回归模型评估抗生素组中年龄和疗效的非线性关联和阈值效应, 阈值通过在预定义区间内寻找使模型似然值最大的转折点来确定。结果: 治疗后, 两组患者的牙周指标均显著改善(P < 0.001)。多因素分析校正混杂因素后发现, 与非抗生素组相比, 抗生素组PD≥5 mm位点百分比减少更显著(β=16.33, 95%CI: 13.40~19.27, P < 0.001)。在抗生素组内, 年龄与疗效存在非线性关系, 以38岁为拐点, ≤38岁的患者疗效显著优于>38岁的患者(P=0.022)。此外, 用药时机显著影响疗效, 在SRP治疗期间(SRP中)使用抗生素的疗效最佳, 优于SRP前或SRP后用药。结论: 在SRP基础上辅助全身应用抗生素, 可进一步改善Ⅲ期和Ⅳ期牙周炎患者的短期临床疗效; 在SRP治疗期间, 对年龄较轻(≤38岁)的患者辅以全身抗生素治疗, 可能取得更好的疗效。
中图分类号:
- R781.42
| 1 |
doi: 10.1111/jcpe.13547 |
| 2 |
邵金龙, 于洋, 吕春旭, 等. 欧洲牙周病学会牙周炎治疗S3级临床指南的介绍与应用解读[J]. 中华口腔医学杂志, 2022, 57(12): 1202- 1208.
|
| 3 |
doi: 10.1902/jop.1989.60.1.67 |
| 4 |
doi: 10.1902/jop.1989.60.7.402 |
| 5 |
doi: 10.1111/prd.12201 |
| 6 |
Herrera D, van Winkelhoff AJ, Matesanz P, et al. Europe's contribution to the evaluation of the use of systemic antimicrobials in the treatment of periodontitis[J/OL]. Periodontol 2000, 2023: prd. 12493(2023-06-14)[2025-10-01]. https://pubmed.ncbi.nlm.nih.gov/37314038/.
|
| 7 |
|
| 8 |
doi: 10.1136/bmjopen-2017-016264 |
| 9 |
|
| 10 |
doi: 10.1111/jcpe.13104 |
| 11 |
|
| 12 |
|
| 13 |
|
| 14 |
杨刚, 闫天行, 胡文杰. 如何做好规范化牙周探诊: 牙周临床基本功训练之三[J]. 中华口腔医学杂志, 2025, 60(6): 678- 684.
|
| 15 |
doi: 10.1111/j.1600-051X.1981.tb02031.x |
| 16 |
doi: 10.1111/j.1600-051X.2006.00905.x |
| 17 |
doi: 10.1002/JPER.20-0764 |
| 18 |
doi: 10.3390/antibiotics9100686 |
| 19 |
doi: 10.1186/s13223-020-00465-7 |
| 20 |
doi: 10.1111/j.1600-051X.1990.tb01072.x |
| 21 |
doi: 10.1111/jcpe.14003 |
| 22 |
doi: 10.1111/jcpe.13096 |
| 23 |
doi: 10.1902/jop.2011.110432 |
| 24 |
|
| 25 |
doi: 10.1016/j.sdentj.2020.04.010 |
| 26 |
doi: 10.1111/jcpe.12427 |
| 27 |
doi: 10.1111/jcpe.12001 |
| 28 |
doi: 10.1902/jop.2007.060437 |
| 29 |
doi: 10.1902/jop.2014.140478 |
| 30 |
doi: 10.1111/j.1600-051X.2010.01632.x |
| 31 |
路瑞芳, 徐莉, 冯向辉, 等. 侵袭性牙周炎基础治疗中不同时机口服抗生素的短期疗效观察[J]. 中华口腔医学杂志, 2012, 47(11): 666- 670.
|
| 32 |
李熠, 徐莉, 路瑞芳, 等. 不同时机口服抗菌药物辅助机械治疗重度慢性牙周炎的临床疗效[J]. 北京大学学报(医学版), 2015, 47(1): 27- 31.
|
| [1] | FarinEbrahimi, 冯志强, FarazEbrahimi, 韩玮华, 于子杨, 贾宽宽, 安金刚. 上颌药物相关性颌骨坏死的不同分期手术治疗效果[J]. 北京大学学报(医学版), 2026, 58(1): 107-114. |
| [2] | 张斯巧, 刘建, 徐涛, 胡文杰, 张浩筠, 危伊萍. 异种骨与人工合成骨在磨牙拔牙同期微翻瓣牙槽嵴保存术中的临床效果比较[J]. 北京大学学报(医学版), 2026, 58(1): 74-83. |
| [3] | 马保金, 李建华, 桑元华, 于洋, 仇吉川, 邵金龙, 李凯, 刘世岳, 杜密, 商玲玲, 葛少华. 基于微环境和干细胞调控的牙周组织再生关键技术的建立与应用[J]. 北京大学学报(医学版), 2025, 57(5): 841-846. |
| [4] | 曹沛, 栾庆先. 牙周炎与全身系统性疾病的思考与探索[J]. 北京大学学报(医学版), 2025, 57(5): 852-858. |
| [5] | 刘相贤, 林毅, 郭金竹. 生物制剂的长期应用对中重度斑块型银屑病患者代谢性生化指标的影响[J]. 北京大学学报(医学版), 2025, 57(5): 934-940. |
| [6] | 包振英, 王雅杰. 炎症指标和细胞因子联合检测在慢性牙周炎中的应用[J]. 北京大学学报(医学版), 2025, 57(4): 772-778. |
| [7] | 石宇彤, 危伊萍, 胡文杰, 徐涛, 张浩筠. 罹患重度牙周炎下颌磨牙拔牙微翻瓣牙槽嵴保存效果评价[J]. 北京大学学报(医学版), 2025, 57(1): 33-41. |
| [8] | 李敬谦, 朱子璐, 焦剑, 施捷. 隐形矫治重度牙周炎患者前牙区病理性移位患牙的临床疗效[J]. 北京大学学报(医学版), 2025, 57(1): 51-56. |
| [9] | 康一帆, 葛严军, 吕晓鸣, 谢尚, 单小峰, 蔡志刚. 即刻种植体支持式义齿修复的血管化髂骨瓣重建下颌骨缺损[J]. 北京大学学报(医学版), 2025, 57(1): 78-84. |
| [10] | 李文菁,张保宙,李恒,赖良鹏,杜辉,孙宁,龚晓峰,李莹,王岩,武勇. 胫距跟融合治疗终末期踝和后足病变的中短期临床结果[J]. 北京大学学报(医学版), 2024, 56(2): 299-306. |
| [11] | 胡玉如,刘娟,李文静,赵亦兵,李启强,路瑞芳,孟焕新. Ⅲ期或Ⅳ期牙周炎患者龈沟液中有机酸浓度与牙周炎的关系[J]. 北京大学学报(医学版), 2024, 56(2): 332-337. |
| [12] | 张晗,秦亦瑄,韦帝远,韩劼. 牙周炎患者种植修复维护治疗依从性的影响因素[J]. 北京大学学报(医学版), 2024, 56(1): 39-44. |
| [13] | 殳畅,韩烨,孙雨哲,杨再目,侯建霞. Ⅲ期牙周炎患者牙周基础治疗前后炎症性贫血相关指标的变化[J]. 北京大学学报(医学版), 2024, 56(1): 45-50. |
| [14] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [15] | 薛蔚,董樑,钱宏阳,费笑晨. 前列腺癌新辅助治疗与辅助治疗的现状及进展[J]. 北京大学学报(医学版), 2023, 55(5): 775-780. |
|
||