北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (2): 234-239. doi: 10.19723/j.issn.1671-167X.2020.02.007
前列腺特异性抗原同源异构体2及其衍生指标在预测前列腺癌病理分级中的价值
- 北京大学第一医院检验科,北京 100034
Clinical value of serum isoform [-2] proprostate-specific antigen and its derivatives in predicting aggressive prostate cancer
Kui-xia SUN,Cun-ling YAN( ),Zhi-yan LI,Ping LIU,Wei ZHANG,Qun HE
),Zhi-yan LI,Ping LIU,Wei ZHANG,Qun HE
- Department of Clinical Laboratory, Peking University First Hospital, Beijing 100034, China
摘要:
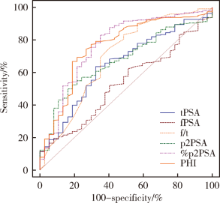
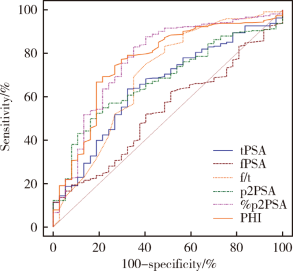
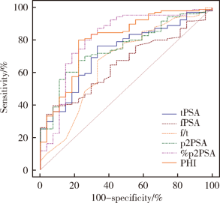
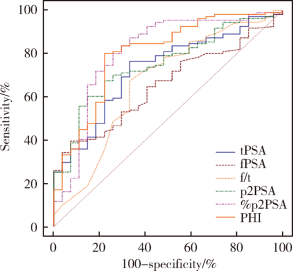
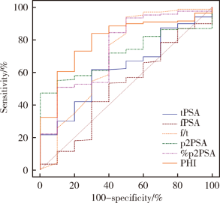
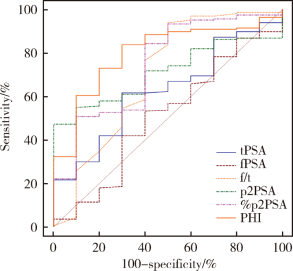
目的 探讨血清前列腺特异性抗原同源异构体2(isoform [-2] proprostate-specific antigen,p2PSA)及经计算得到的%p2PSA和前列腺健康指数(prostate health index,PHI)等指标预测前列腺癌(prostate cancer, PCa)病理分级的价值.方法: 回顾性入组了322例来自北京大学第一医院在2015年8月至2018年5月期间就诊的PCa患者,其中143例为进行经直肠超声引导的前列腺穿刺活检证实的PCa患者,179例为进行PCa根治术的患者.采用全自动免疫分析仪DxI800检测患者的术前预留血清中前列腺特异性抗原(total prostate-specific antigen,tPSA),游离前列腺抗原(free prostate antigen,fPSA),fPSA/tPSA比值(f/t),p2PSA水平,并计算得到%p2PSA 和PHI,以术后病理结果确定Gleason评分,采用受试者工作曲线(receiver operating characteristic curve,ROC)比较p2PSA,%p2PSA及PHI与传统指标tPSA,fPSA和f/t预测高级别前列腺癌(Gleason评分≥7)的价值.结果: Gleason评分≥7患者的p2PSA,%p2PSA和 PHI的中位数水平均高于Gleason评分<7患者(p2PSA: 30.22 ng/L vs. 18.33 ng/L; %p2PSA: 2.50 vs. 1.27; PHI: 91.81 vs. 35.44; P值均<0.01).%p2PSA和PHI预测高级别PCa的曲线下面积(area under curve,AUC)为0.770和0.760,高于传统指标tPSA,fPSA和f/t(AUC分别为0.648,0.536和 0.693).进行前列腺穿刺术证实为PCa的患者中,PHI和%p2PSA预测高级别PCa的价值(AUC分别为0.801和0.808)明显高于tPSA,fPSA和f/t(AUC分别为0.729,0.655和0.665).进行PCa根治术后的患者中,PHI 和%p2PSA预测高级别PCa的价值(AUC分别为 0.798和0.744)也有高于其他传统指标tPSA,fPSA和f/t (AUC分别为0.625, 0.507和0.697)的趋势.结论: 与传统指标tPSA,fPSA和f/t相比,p2PSA的衍生指标%p2PSA和PHI对于高级别PCa具有更高的预测价值,可以帮助临床评估PCa治疗方案,为患者及时制定更合适的诊疗策略.
中图分类号:
- R737.2
| [1] | Stephan C, Vincendeau S, Houlgatte A , et al. Multicenter evaluation of [-2]proprostate-specific antigen and the prostate health index for detecting prostate cancer[J]. Clin Chem, 2013,59(1):306-314. |
| [2] | 黄宜, 王文涓, 许静 , 等. p2PSA及其相关指标 PHI 在前列腺癌诊断中的应用价值[J]. 检验医学, 2019,34(7):600-604. |
| [3] | Quinn D, Gross M . Show us a sign: the search for "game changing" prostate cancer biomarkers[J]. Lancet Oncol, 2011,12(3):204-206. |
| [4] | Vukovic I, Djordjevic D, Bojanic N , et al. Predictive value of [-2]propsa(p2psa) and its derivatives for the prostate cancer detection in the 2.0 to 10.0 ng/mL PSA range[J]. Int Braz J Urol, 2017,43(1):48-56. |
| [5] | 朱耀, 唐钵, 戴波 , 等. 前列腺健康指数在中国男性前列腺癌诊断中的应用研究[J]. 中华外科杂志, 2017,55(10):734-737. |
| [6] | 闫存玲, 李志艳, 何群 , 等. 血清前列腺特异性抗原同源异构体-2在前列腺癌中的应用价值[J]. 中华检验医学杂志, 2015,38(12):813-817. |
| [7] | Catalona WJ, Partin AW, Sanda MG , et al. A multicenter study of [-2]pro-prostate specific antigen combined with prostate speci-fic antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0 ng/ml prostate specific antigen range[J]. J Urol, 2011,185(5):1650-1655. |
| [8] | Jansen FH, van Schaik RHN, Kurstjens J , et al. Prostate-specific antigen (PSA) isoform p2PSA in combination with total PSA and free PSA improves diagnostic accuracy in prostate cancer detection[J]. Eur Urol, 2010,57(6):921-927 |
| [9] | Fossati N, Buffi NM, Haese A , et al. Preoperative prostate speci-fic antigen isoform p2PSA and its derivatives, %p2PSA and prostate health index, predict pathologic outcomes in patients undergoing radical prostatectomy for prostate cancer: results from a multicentric European prospective study[J]. Eur Urol, 2015,68(1):132-138 |
| [10] | Eminaga O, Bögemann M, Breil B , et al. Preoperative prostate-specific antigen isoform p2PSA ≤ 22.5 pg/ml predicts advanced prostate cancer in patients undergoing radical prostatectomy[J]. Urol Oncol, 2014,32(8):1117-1126. |
| [11] | Guazzoni G, Lazzeri M, Nava L , et al. Preoperative prostate-specific antigen isoform p2PSA and its derivatives, %p2PSA and prostate health index, predict pathologic outcomes in patients undergoing radicalprostatectomy for prostate cancer[J]. Eur Urol, 2012,61(3):455-466. |
| [12] | Schwen ZR, Tosoian JJ, Sokoll LJ , et al. Prostate Health Index (PHI) Predicts High-stage Pathology in African American Men[J]. Urology, 2016,90:136-140. |
| [13] | Dolejsova O, Kucera R, Fuchsova R , et al. The ability of Prostate Health Index (PHI) to predict gleason score in patients with prostate cancer and discriminate patients between gleason score 6 and gleason score higher than 6: a study on 320 patients after radical prostatectomy[J]. Technol Cancer Res Treat, 2018,17:1-6. |
| [14] | Chiu PK, Lai FM, Teoh JY , et al. Prostate health index and %p2PSA predict aggressive prostate cancer pathology in Chinese[J]. Ann Surg Onclo, 2016,23(8):2707-2714. |
| [15] | 王友林, 朱磊一, 姜波 , 等. 超声引导下经直肠前列腺穿刺与前列腺癌根治术后病理组织Gleason评分差异性的研究[J]. 临床泌尿外科杂志, 2015,30(7):628-630. |
| [1] | 于书慧,韩佳凝,钟丽君,陈聪语,肖云翔,黄燕波,杨洋,车新艳. 术前盆底肌电生理参数对前列腺癌根治性切除术后早期尿失禁的预测价值[J]. 北京大学学报(医学版), 2024, 56(4): 594-599. |
| [2] | 颜野,李小龙,夏海缀,朱学华,张羽婷,张帆,刘可,刘承,马潞林. 前列腺癌根治术后远期膀胱过度活动症的危险因素[J]. 北京大学学报(医学版), 2024, 56(4): 589-593. |
| [3] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [4] | 黄教悌,胡菁,韩博. 治疗相关神经内分泌前列腺癌机制研究与靶向治疗新进展[J]. 北京大学学报(医学版), 2024, 56(4): 557-561. |
| [5] | 刘圣杰,侯惠民,吕政通,丁鑫,王璐,张磊,刘明. 双极雄激素序贯免疫检查点抑制剂治疗转移性去势抵抗性前列腺癌4例[J]. 北京大学学报(医学版), 2022, 54(4): 766-769. |
| [6] | 白杲琛,宋毅,金杰,虞巍,何志嵩. 多西他赛联合卡铂治疗转移性去势抵抗性前列腺癌的临床疗效[J]. 北京大学学报(医学版), 2021, 53(4): 686-691. |
| [7] | 徐涛,韩敬丽,姚伟娟. 雄激素剥夺治疗相关心血管疾病的机制与临床对策[J]. 北京大学学报(医学版), 2020, 52(4): 607-609. |
| [8] | 李文卿,任思楣,龙星博,田雨青. 棕榈酰化蛋白质组学分析揭示前列腺癌细胞中雄激素促进代谢相关蛋白棕榈酰化修饰[J]. 北京大学学报(医学版), 2020, 52(2): 227-233. |
| [9] | 张宽根,周雨禾,邵雅昆,梅放,由江峰,刘北英,裴斐. 肿瘤转移抑制基因LASS2/TMSG1 S248A突变体通过增加ATP6V0C表达促进前列腺癌的侵袭[J]. 北京大学学报(医学版), 2019, 51(2): 210-220. |
| [10] | 唐旭,赵卫红,宋琴琴,殷华奇,杜依青,盛正祚,王强,张晓威,李清,刘士军,徐涛. SOX10对前列腺癌细胞增殖及侵袭的影响[J]. 北京大学学报(医学版), 2018, 50(4): 602-606. |
| [11] | 邹鹏程,杨一峰,徐晓艳,刘北英,梅放,由江峰,刘启忱,裴斐 . 沉默液泡型ATP酶c亚基ATP6V0C抑制人前列腺癌细胞侵袭的分子机制[J]. 北京大学学报(医学版), 2017, 49(6): 937-947. |
| [12] | 纪光杰,黄聪,宋刚,李学松,宋毅,周利群. 去势抵抗性前列腺癌进展时间的预测因素分析[J]. 北京大学学报(医学版), 2017, 49(4): 657-662. |
| [13] | 杨恺惟, 虞巍, 宋毅, 黄立华, 韩文科, 何志嵩, 金杰, 周利群. 影响多西他赛联合泼尼松治疗转移性去势抵抗性前列腺癌疗效的因素分析[J]. 北京大学学报(医学版), 2015, 47(4): 592-596. |
| [14] | 刘汀, 王霄英, 王义. 用Cox模型对前列腺癌相关临床检查的多因素生存分析[J]. 北京大学学报(医学版), 2009, 41(2): 184-187. |
| [15] | 尚永丰. 核受体对基因转录的调控[J]. 北京大学学报(医学版), 2002, 34(5): 440-450. |
|
||