北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (1): 136-144. doi: 10.19723/j.issn.1671-167X.2019.01.024
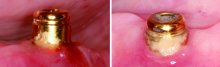
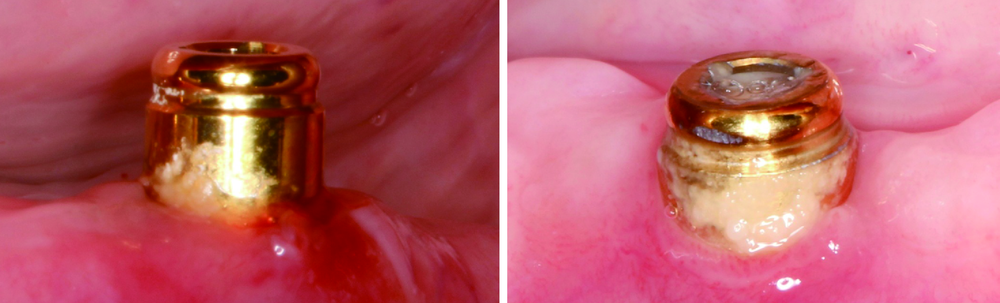
无牙颌患者locator附着体种植覆盖义齿修复后口腔卫生维护的纵向研究
刘潇倩1,陈秋雯1,冯海兰1,王兵2,屈健2,孙振2,衡墨迪2,潘韶霞1,△( )
)
- 1. 北京大学口腔医学院·口腔医院, 修复科, 北京 100081
2. 义齿加工中心, 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室, 北京 100081
Oral hygiene maintenance of locator attachments implant overdentures in edentulous population: A longitudinal study
Xiao-qian LIU1,Qiu-wen CHEN1,Hai-lan FENG1,Bing WANG2,Jian QU2,Zhen SUN2,Mo-di HENG2,Shao-xia PAN1,△( )
)
- 1. Department of Prosthodontics, Beijing 100081, China
2. Department Laboratory, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
目的:调查无牙颌患者locator附着体种植覆盖义齿修复后口腔卫生维护状况,分析其口腔卫生维护行为、卫生状况与种植体周围软硬组织健康的相关性。方法:纳入2012年1月至2016年5月于北京大学口腔医院修复科接受locator附着体种植覆盖义齿修复的无牙颌患者,复查时记录种植体周围病的发生情况、改良菌斑指数(modified plaque index, mPLI)、探诊出血指数(sulcus bleeding index, SBI)、牙龈指数(gingival index, GI)、探诊深度(probing depth, PD)等,并利用X线平行投照法观察边缘骨吸收,同时调查患者对附着体的日常清洁行为。分析患者的口腔卫生维护行为、卫生状况与种植体周围病发生率的关系。结果:共纳入50名患者(125枚种植体),平均随访了22个月(6~54个月),平均mPLI、SBI、GI分别为1.4±1.2、0.8±0.7、0.7±0.6,PD为(2.2±0.7) mm,近远中边缘骨吸收分别为(1.1±1.1) mm、(0.9±0.9) mm。种植体周围黏膜炎的发生率为49.6%,种植体周围炎的发生率为0。口腔卫生差(mPLI≥2)的患者种植体周围黏膜炎的发生率是口腔卫生良好者(mPLI<1)的11.9倍,每日清洁附着体两次及以上的患者mPLI得分显著低于清洁次数不足两次的患者(P<0.05)。结论:无牙颌患者种植locator附着体种植覆盖义齿修复后的口腔卫生维护不足,口腔卫生维护不良与无牙颌患者种植体周围黏膜炎的发生相关,口腔卫生差的患者种植体发生黏膜炎的风险是口腔卫生良好者的11.9倍,附着体的清洁是患者应关注的重点内容。
中图分类号:
- R783.4
| [1] |
Lindhe J, Meyle J . Peri-implant diseases: Consensus report of the sixth European Workshop on periodontology[J]. J Clin Periodontol, 2008,35(8 Suppl):282-285.
doi: 10.1111/j.1600-051X.2008.01278.x pmid: 18724855 |
| [2] |
Heitz-Mayfield LJ . Peri-implant diseases: diagnosis and risk indicators[J]. J Clin Periodontol, 2008,35(8 Suppl):292-304.
doi: 10.1111/j.1600-051X.2008.01275.x pmid: 18724857 |
| [3] |
Laine ML, Leonhardt A, Roos-Jansåker AM , et al. IL-1RN gene polymorphism is associated with peri-implantitis[J]. Clin Oral Implants Res, 2006,17(4):380-385.
doi: 10.1111/j.1600-0501.2006.01249.x pmid: 16907768 |
| [4] |
Heitz-Mayfield LJ . Disease progression: identification of high-risk groups and individuals for periodontitis[J]. J Clin Periodontol, 2005,32(Suppl 6):196-209.
doi: 10.1111/j.1600-051X.2005.00803.x pmid: 16128838 |
| [5] |
Ericsson I, Berglundh T, Marinello C , et al. Long-standing plaque and gingivitis at implants and teeth in the dog[J]. Clin Oral Implants Res, 1992,3(3):99-103.
doi: 10.1034/j.1600-0501.1992.030301.x pmid: 1290796 |
| [6] |
Pontoriero R, Tonelli MP, Carnevale G , et al. Experimentally induced peri-implant mucositis. A clinical study in humans[J]. Clin Oral Implants Res, 1994,5(4):254-259.
doi: 10.1034/j.1600-0501.1994.050409.x pmid: 7640340 |
| [7] |
Salvi GE, Aglietta M, Eick S , et al. Reversibility of experimental peri-implant mucositis compared with experimental gingivitis in humans[J]. Clin Oral Implants Res, 2012,23(2):182-190.
doi: 10.1111/j.1600-0501.2011.02220.x pmid: 21806683 |
| [8] |
Salvi GE, Ramseier CA . Efficacy of patient-administered mecha-nical and/or chemical plaque control protocols in the management of peri-implant mucositis. A systematic review[J]. J Clin Perio-dontol, 2015,42(Suppl 16):S187-S201.
doi: 10.1111/jcpe.12321 pmid: 25495416 |
| [9] |
Todescan S, Lavigne S, Kelekis-Cholakis A . Guidance for the maintenance care of dental implants: clinical review[J]. J Can Dent Assoc, 2012,78:c107.
doi: 10.1111/j.1752-7325.2011.00311.x pmid: 23306040 |
| [10] |
Tawse-Smith A, Duncan WJ, Payne AG , et al. Relative effectiveness of powered and manual toothbrushes in elderly patients with implant-supported mandibular overdentures[J]. J Clin Periodontol, 2002,29(4):275-280.
doi: 10.1034/j.1600-051X.2002.290401.x pmid: 11966923 |
| [11] | Budtz-Jorgensen E . Prosthodontics for the elderly: Diagnosis and treatment[M]. Chicago: Quintessence, 1999. |
| [12] |
Mombelli A, van Oosten MA, Schurch EJ , et al. The microbiota associated with successful or failing osseointegrated titanium implants[J]. Oral Microbiol Immunol, 1987,2(4):145-151.
doi: 10.1111/j.1399-302X.1987.tb00298.x |
| [13] |
Loe H, Silness J . Periodontal disease in pregnancy. I. Prevalence and severity[J]. Acta Odontol Scand, 1963,21:533-551.
doi: 10.3109/00016356309011240 pmid: 14121956 |
| [14] |
Renvert S, Persson GR, Pirih FQ , et al. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations[J]. J Periodontol, 2018,89(Suppl 1):S304-S312.
doi: 10.1002/JPER.17-0588 |
| [15] |
Meijer HJA, Raghoebar GM, Batenburg RHK , et al. Mandibular overdentures supported by two Brånemark, IMZ or ITI implants: a ten-year prospective randomized study[J]. J Clin Periodontol, 2009,36(9):799-806.
doi: 10.1111/j.1600-051X.2009.01442.x |
| [16] |
Elsyad MA, Elsaih EA, Khairallah AS . Marginal bone resorption around immediate and delayed loaded implants supporting a locator-retained mandibular overdenture. A 1-year randomised controlled trial[J]. J Oral Rehabil, 2014,41(8):608-618.
doi: 10.1111/joor.12182 pmid: 24814408 |
| [17] |
di Torresanto VM, Milinkovic I, Torsello F , et al. Computer-assisted flapless implant surgery in edentulous elderly patients: a 2-year follow up[J]. Quintessence Int, 2014,45(5):419-429.
doi: 10.3290/j.qi.a31534 pmid: 24634906 |
| [18] |
胡秀莲, 罗佳, 李健慧 , 等. 无牙颌种植修复患者127例临床回顾研究[J]. 中华口腔医学杂志, 2014,49(6):333-338.
doi: 10.3760/cma.j.issn.1002-0098.2014.06.004 |
| [19] |
Meijer HJ, Raghoebar GM, de Waal YC ,et al. Incidence of peri-implant mucositis and peri-implantitis in edentulous patients with an implant-retained mandibular overdenture during a 10-year follow-up period[J]. J Clin Periodontol, 2014,41(12):1178-1183.
doi: 10.1111/jcpe.12311 pmid: 25229397 |
| [20] |
Roos-Jansaker AM, Renvert H, Lindahl C , et al. Nine- to fourteen-year follow-up of implant treatment. Part Ⅲ: factors associated with peri-implant lesions[J]. J Clin Periodontol, 2006,33(4):296-301.
doi: 10.1111/cpe.2006.33.issue-4 |
| [21] |
Ferreira SD, Silva GL, Cortelli JR , et al. Prevalence and risk variables for peri-implant disease in Brazilian subjects[J]. J Clin Periodontol, 2006,33(12):929-935.
doi: 10.1111/cpe.2006.33.issue-12 |
| [22] |
Zitzmann NU, Berglundh T, Marinello CP , et al. Experimental peri-implant mucositis in man[J]. J Clin Periodontol, 2001,28(6):517-523.
doi: 10.1034/j.1600-051x.2001.028006517.x pmid: 11350518 |
| [23] |
Costa FO, Takenaka-Martinez S, Cota LO , et al. Peri-implant disease in subjects with and without preventive maintenance: a 5-year follow-up[J]. J Clin Periodontol, 2012,39(2):173-181.
doi: 10.1111/j.1600-051X.2011.01819.x pmid: 22111654 |
| [24] |
Ogata Y, Nakayama Y, Tatsumi J , et al. Prevalence and risk factors for peri-implant diseases in Japanese adult dental patients[J]. J Oral Sci, 2016,59(1):1-11.
doi: 10.2334/josnusd.16-0027 pmid: 27725369 |
| [25] |
D’Hoedt B, Schulte W . A comparative study of results with various endosseous implant systems[J]. Int J Oral Maxillofac Implants, 1989,4(2):95-105.
pmid: 2599587 |
| [26] |
Versteegh PA, van Beek GJ, Slagter AP , et al. Clinical evaluation of mandibular overdentures supported by multiple-bar fabrication: a follow-up study of two implant systems[J]. Int J Oral Maxillofac Implants, 1995,10(5):595-603.
pmid: 7591005 |
| [27] |
Kirsch A, Mentag PJ . The IMZ endosseous two phase implant system: a complete oral rehabilitation treatment concept[J]. J Oral Implantol, 1986,12(4):576-589.
pmid: 3540314 |
| [28] |
Smith DE, Zarb GA . Criteria for success of osseointegrated endosseous implants[J]. J Prosthet Dent, 1989,62(5):567-572.
doi: 10.1016/0022-3913(89)90081-4 pmid: 2691661 |
| [29] |
Esposito M, Hirsch JM, Lekholm U , et al. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis[J]. Eur J Oral Sci, 1998,106(3):721-764.
doi: 10.1046/j.0909-8836..t01-6-.x |
| [30] |
Pjetursson BE, Helbling C, Weber HP , et al. Peri-implantitis susceptibility as it relates to periodontal therapy and supportive care[J]. Clin Oral Implants Res, 2012,23(7):888-894.
doi: 10.1111/j.1600-0501.2012.02474.x pmid: 22530771 |
| [31] |
Cho-Yan LJ, Mattheos N, Nixon KC , et al. Residual periodontal pockets are a risk indicator for peri-implantitis in patients treated for periodontitis[J]. Clin Oral Implants Res, 2012,23(3):325-333.
doi: 10.1111/j.1600-0501.2011.02264.x pmid: 22020202202020220 |
| [32] |
Karoussis IK, Salvi GE, Heitz-Mayfield LJ , et al. Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System[J]. Clin Oral Implants Res, 2003,14(3):329-339.
doi: 10.1034/j.1600-0501.000.00934.x |
| [33] |
Mombelli A, Marxer M, Gaberthuel T , et al. The microbiota of osseointegrated implants in patients with a history of periodontal disease[J]. J Clin Periodontol, 1995,22(2):124-130.
doi: 10.1111/j.1600-051X.1995.tb00123.x pmid: 7775668 |
| [34] |
张海东, 孟焕新 . 牙周状况及牙周治疗对口腔种植修复长期效果的影响[J]. 中华口腔医学杂志, 2013,48(4):229-232.
doi: 10.3760/cma.j.issn.1002-0098.2013.04.009 |
| [35] |
Quirynen M, van Assche N . Microbial changes after full-mouth tooth extraction, followed by 2-stage implant placement[J]. J Clin Periodontol, 2011,38(6):581-589.
doi: 10.1111/j.1600-051X.2011.01728.x pmid: 21488934 |
| [36] |
Teughels W, van Eldere J, van Steenberghe D , et al. Influence of nicotine and cotinine on epithelial colonization by periodontopathogens[J]. J Periodontol, 2005,76(8):1315-1322.
doi: 10.1902/jop.2005.76.8.1315 pmid: 16101364 |
| [37] | Huang R, Li M, Gregory RL . Effect of nicotine on growth and metabolism of Streptococcus mutans[J]. Eur J Oral Sci, 2012,120(4):319-325. |
| [38] |
Li M, Huang R, Zhou X , et al. Effect of nicotine on dual-species biofilms of Streptococcus mutans and Streptococcus sanguinis[J]. FEMS Microbiol Lett, 2014,350(2):125-132.
doi: 10.1111/1574-6968.12317 pmid: 24164376 |
| [39] |
Barao VA, Ricomini-Filho AP, Faverani LP , et al. The role of nicotine, cotinine and caffeine on the electrochemical behavior and bacterial colonization to cp-Ti[J]. Mater Sci Eng C Mater Biol Appl, 2015,56:114-124.
doi: 10.1016/j.msec.2015.06.026 pmid: 26249572 |
| [40] |
Mombelli A, Muller N, Cionca N . The epidemiology of peri-implantitis[J]. Clin Oral Implants Res, 2012,23(Suppl 6):67-76.
doi: 10.1111/clr.12027 pmid: 23062130 |
| [41] |
Vervaeke S, Collaert B, Cosyn J , et al. A multifactorial analysis to identify predictors of implant failure and peri-implant bone loss[J]. Clin Implant Dent Relat Res, 2015,17(Suppl 1):e298-e307.
doi: 10.1111/cid.12149 pmid: 24004332 |
| [42] |
Strietzel FP, Reichart PA, Kale A , et al. Smoking interferes with the prognosis of dental implant treatment: a systematic review and meta-analysis[J]. J Clin Periodontol, 2007,34(6):523-544.
doi: 10.1111/j.1600-051X.2007.01083.x pmid: 17509093 |
| [43] |
Zimmermann H, Zimmermann N, Hagenfeld D , et al. Is frequency of tooth brushing a risk factor for periodontitis? A systematic review and meta-analysis[J]. Community Dentistry and Oral Epidemiology, 2015,43(2):116-127.
doi: 10.1111/cdoe.12126 pmid: 25255820 |
| [44] |
Elsyad MA . Patient satisfaction and prosthetic aspects with mini-implants retained mandibular overdentures. A 5-year prospective study[J]. Clin Oral Implants Res, 2016,27(7):926-933.
doi: 10.1111/clr.12660 pmid: 26129836 |
| [45] |
Cordaro L, di Torresanto VM, Petricevic N , et al. Single unit attachments improve peri-implant soft tissue conditions in mandibular overdentures supported by four implants[J]. Clin Oral Implants Res, 2013,24(5):536-542.
doi: 10.1111/j.1600-0501.2012.02426.x pmid: 22320359 |
| [46] |
Walton JN , MacEntee MI. Problems with prostheses on implants: a retrospective study[J]. J Prosthet Dent, 1994,71(3):283-288.
doi: 10.1016/0022-3913(94)90468-5 pmid: 8164171 |
| [1] | 王聪伟,高敏,于尧,章文博,彭歆. 游离腓骨瓣修复下颌骨缺损术后义齿修复的临床分析[J]. 北京大学学报(医学版), 2024, 56(1): 66-73. |
| [2] | 丁茜,李文锦,孙丰博,谷景华,林元华,张磊. 表面处理对氧化钇和氧化镁稳定的氧化锆种植体晶相及断裂强度的影响[J]. 北京大学学报(医学版), 2023, 55(4): 721-728. |
| [3] | 孙菲,刘建,李思琪,危伊萍,胡文杰,王翠. 种植体黏膜下微生物在健康种植体和种植体周炎中的构成与差异:一项横断面研究[J]. 北京大学学报(医学版), 2023, 55(1): 30-37. |
| [4] | 梁峰,吴敏节,邹立东. 后牙区单牙种植修复5年后的临床修复疗效观察[J]. 北京大学学报(医学版), 2021, 53(5): 970-976. |
| [5] | 孙玉春,王勇,邓珂慧,陈虎,李伟伟,赵一姣,潘韶霞,叶红强,周永胜. 功能易适数字化全口义齿的自主创新研发[J]. 北京大学学报(医学版), 2020, 52(2): 390-394. |
| [6] | 游浪,邓珂慧,李伟伟,赵一姣,孙玉春,周永胜. 无牙颌患者鼻唇角变化侧面观的视觉敏感阈值[J]. 北京大学学报(医学版), 2020, 52(1): 107-112. |
| [7] | 曹悦,陈俊锴,邓珂慧,王勇,孙玉春,赵一姣. 三款口内三维扫描仪获取无牙颌红膏初印模精度的对比评价[J]. 北京大学学报(医学版), 2020, 52(1): 129-137. |
| [8] | 释栋,曹婕,戴世爱,孟焕新. 植体周炎再生治疗短期疗效观察[J]. 北京大学学报(医学版), 2020, 52(1): 58-63. |
| [9] | 林春平,卢松鹤,朱浚鑫,胡洪成,岳兆国,唐志辉. 个性化根形种植体的螺纹形态对周围牙槽骨应力分布影响的三维有限元分析[J]. 北京大学学报(医学版), 2019, 51(6): 1130-1137. |
| [10] | 吴敏节,邹立东,梁峰. 上前牙即刻种植即刻修复负载3年后软、硬组织变化的临床观察[J]. 北京大学学报(医学版), 2018, 50(4): 694-699. |
| [11] | 刘婧寅,陈飞,葛严军,魏菱,潘韶霞,冯海兰. 选择性激光熔化种植体对早期骨矿化沉积率的影响[J]. 北京大学学报(医学版), 2018, 50(1): 117-122. |
| [12] | 王晶,和璐. 自我机械清除舌苔对舌苔源性口臭患者口臭程度的影响[J]. 北京大学学报(医学版), 2017, 49(2): 344-348. |
| [13] | 梁乃文,石磊,黄颖,邓旭亮. 不同形貌纯钛表面对人脐静脉内皮细胞生物学行为的影响[J]. 北京大学学报(医学版), 2017, 49(1): 43-048. |
| [14] | 李贝贝, 林野, 崔宏燕, 郝强, 胥加斌, 邸萍. 碳纤维增强“All-on-4”即刻修复体的临床评价[J]. 北京大学学报(医学版), 2016, 48(1): 133-137. |
| [15] | 崔宏燕, 邸萍, 李健慧, 林野, 刘蓉蓉. 电火花蚀刻技术在种植修复体制作中的应用[J]. 北京大学学报(医学版), 2015, 47(2): 336-339. |
|
||