北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (4): 628-631. doi: 10.19723/j.issn.1671-167X.2019.04.005
肾癌术后局部复发患者的临床病理特征及预后分析
唐琦,林榕城,姚林,张争,郝瀚,张崔建,蔡林,李学松,何志嵩( ),周利群(
),周利群( )
)
- 北京大学第一医院泌尿外科,北京大学泌尿外科研究所, 北京 100034
Clinicopathologic features and prognostic analyses of locally recurrent renal cell carcinoma patients after initial surgery
Qi TANG,Rong-cheng LIN,Lin YAO,Zheng ZHANG,Han HAO,Cui-jian ZHANG,Lin CAI,Xue-song LI,Zhi-song HE( ),Li-qun ZHOU(
),Li-qun ZHOU( )
)
- Department of Urology, Peking University First Hospital; Institute of Urology, Peking University, Beijing 100034, China
摘要:
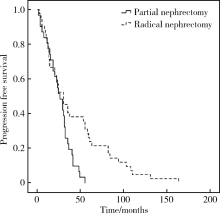
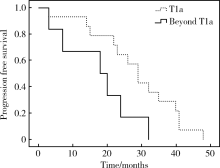
目的:探讨肾癌术后局部复发患者的临床病理特征及可能的预后影响因素。方法:肾癌术后局部复发包括残留肾脏、肾窝、腹壁、同侧肾上腺及同侧腹膜后淋巴结的复发病灶。回顾性分析自2006年1月至2018年6月于北京大学第一医院泌尿外科接受手术治疗的81例肾癌术后局部复发患者资料,收集患者两次手术治疗的临床及病理资料,进行对比统计分析。结果:研究共纳入81名患者,其中43例在北京大学第一医院接受初次手术治疗,38例于外院接受手术治疗。初次手术时38例(本院26例,外院12例)患者接受肾部分切除,43例(本院17例,外院26例)患者接受根治性肾切除。总体中位复发时间为26个月(3~164个月), 其中肾部分切除患者中位复发时间26个月(3~55个月),根治性肾切除患者中位复发时间30个月(4~164个月), P=0.009。69例患者为单一部位复发,其中残留肾脏复发29例,肾窝复发20例,腹壁复发4例,同侧淋巴结复发5例,同侧肾上腺复发11例,另外12例患者为多部位复发。78例患者接受完整手术切除,3例患者接受射频消融治疗。复发病灶病理透明细胞癌72例,乳头状细胞癌8例(Ⅰ型7例,Ⅱ型1例), Xp11易位性肾癌1例。43例于北京大学第一医院行初次手术的患者具有完整初次手术病理资料,其中17例患者行根治性肾切除术,病理分期T1a期4例,T1b期2例,T2a期1例,T3a期8例,T3b期2例,另外26例患者行肾部分切除,病理分期T1a期18例,T1b期7例,T3a期1例。肾部分切除患者中T1a期患者中位复发时间长于T1a期以上患者(29个月 vs. 18个月,P=0.041)。末次随访时存活患者58例,死亡4例,失访19例。3年无瘤生存率为81.9%, 5年无瘤生存率为53.6%。结论:肾部分切除患者术后中位局部复发时间短于肾根治切除患者,初次手术肾部分切除病理分期T1a患者中位复发时间长于T1a以上分期患者,复发病灶可进行完整切除患者,二次术后可获得较长时间生存。
中图分类号:
- R737.11
| [1] | Siegel R, Miller K, Jemal A . Cancer statistics, 2018[J]. CA Cancer J Clin, 2018,68(1):7-30. |
| [2] | Kuusk T , Grivas N, de Bruijn R, et al. The current management of renal cell carcinoma[J]. Minerva Med, 2017,108(4):357-369. |
| [3] | Margulis V, Mcdonald M, Tamboli P , et al. Predictors of oncolo-gical outcome after resection of locally recurrent renal cell carcinoma[J]. J Urol, 2009,181(5):2044-2051. |
| [4] | 杨洋, 肖云翔, 周利群 , 等. 手术治疗肾癌根治术后孤立局部复发病灶的长期预后分析[J]. 北京大学学报(医学版), 2014,46(4):528-531. |
| [5] | Lane BR, Gill IS . 5-year outcomes of laparoscopic partial nephrectomy[J]. J Urol, 2007,177(1):70-74. |
| [6] | Campbell SC, Novick AC . Management of local recurrence fol-lowing radical nephrectomy or partial nephrectomy[J]. Urol Clin North Am, 1994,21(4):593-599. |
| [7] | Bigot P, Hetet JF, Bernhard JC , et al. Nephron-sparing surgery for renal tumors measuring more than 7 cm: morbidity, and functional and oncological outcomes[J]. Clin Genitourin Cancer, 2014,12(1):e19-e27. |
| [8] | Mir MC, Derweesh I, Porpiglia F , et al. Partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: a systematic review and meta-analysis of comparative studies[J]. Eur Urol, 2017,71(4):606-617. |
| [9] | Brookman-May S, May M, Shariat SF , et al. Features associated with recurrence beyond 5 years after nephrectomy and nephron-sparing surgery for renal cell carcinoma: development and internal validation of a risk model (PRELANE score) to predict late recurrence based on a large multicenter database (CORONA/SATURN Project)[J]. Eur Urol, 2013,64(3):472-477. |
| [10] | Nakano E, Fujioka H, Matsuda M , et al. Late recurrence of renal cell carcinoma after nephrectomy[J]. Eur Urol, 1984,10(5):347-349. |
| [11] | Miyao N, Naito S, Ozono S , et al. Late recurrence of renal cell carcinoma: retrospective and collaborative study of the Japanese Society of Renal Cancer[J]. Urology, 2011,77(2):379-384. |
| [12] | Park YH, Baik KD, Lee YJ , et al. Late recurrence of renal cell carcinoma >5 years after surgery: clinicopathological characteristics and prognosis[J]. BJU Int, 2012,110(11 Pt B):E553-E558. |
| [13] | Lee BH, Feifer A, Feuerstein MA , et al. Validation of a post-operative nomogram predicting recurrence in patients with conventional clear cell renal cell carcinoma[J]. Eur Urol Focus, 2018,4(1):100-105. |
| [14] | Itano NB, Blute ML, Spotts B , et al. Outcome of isolated renal cell carcinoma fossa recurrence after nephrectomy[J]. J Urol, 2000,164(2):322-325. |
| [15] | Yohannan J, Feng T, Berkowitz J , et al. Laparoscopic resection of local recurrence after previous radical nephrectomy for clinically localized renal-cell carcinoma: perioperative outcomes and initial observations[J]. J Endourol, 2010,24(10):1609-1612. |
| [16] | Ljungberg B, Albiges L, Abu-Ghanem Y , et al. European Association of Urology Guidelines on Renal Cell Carcinoma: The 2019 Update[J]. Eur Urol, 2019,75(5):799-810. |
| [1] | 张树栋,谢睿扬. 机器人手术时代的肾癌合并腔静脉瘤栓治疗策略[J]. 北京大学学报(医学版), 2024, 56(4): 562-564. |
| [2] | 舒帆,郝一昌,张展奕,邓绍晖,张洪宪,刘磊,王国良,田晓军,赵磊,马潞林,张树栋. 肾部分切除术治疗囊性肾癌的功能学和肿瘤学结果:单中心回顾性研究[J]. 北京大学学报(医学版), 2024, 56(4): 667-672. |
| [3] | 兰东,刘茁,李宇轩,王国良,田晓军,马潞林,张树栋,张洪宪. 根治性肾切除和静脉癌栓取出术大出血的危险因素[J]. 北京大学学报(医学版), 2023, 55(5): 825-832. |
| [4] | 陈斌,吴超,刘彬,于涛,王振宇. 脊髓髓内海绵状血管瘤患者不同治疗方式的预后[J]. 北京大学学报(医学版), 2023, 55(4): 652-657. |
| [5] | 王跃,张爽,张虹,梁丽,徐玲,程元甲,段学宁,刘荫华,李挺. 激素受体阳性/人表皮生长因子受体2阴性乳腺癌临床病理特征及预后[J]. 北京大学学报(医学版), 2022, 54(5): 853-862. |
| [6] | 秦彩朋,宋宇轩,丁梦婷,王飞,林佳兴,杨文博,杜依青,李清,刘士军,徐涛. 肾癌免疫治疗疗效评估突变预测模型的建立[J]. 北京大学学报(医学版), 2022, 54(4): 663-668. |
| [7] | 刘茁,朱国栋,唐世英,洪鹏,赵勋,张启鸣,李丽伟,彭冉,陈志刚,王滨帅,张丽,杨飞龙,葛力源,孙争辉,张树栋,王国良,田晓军,张洪宪,马潞林. 外科手术治疗年龄≥75岁的高龄肾细胞癌合并静脉癌栓患者的临床经验[J]. 北京大学学报(医学版), 2022, 54(4): 774-778. |
| [8] | 王薇,蔡林,高莹,郭晓蕙,张俊清. 原发性醛固酮增多症术后持续性重度高钾血症1例[J]. 北京大学学报(医学版), 2022, 54(2): 376-380. |
| [9] | 洪鹏,田晓军,赵小钰,杨飞龙,刘茁,陆敏,赵磊,马潞林. 肾移植术后双侧乳头状肾癌1例[J]. 北京大学学报(医学版), 2021, 53(4): 811-813. |
| [10] | 肖若陶,刘承,徐楚潇,何为,马潞林. 术前血小板参数与局部进展期肾细胞癌预后[J]. 北京大学学报(医学版), 2021, 53(4): 647-652. |
| [11] | 于焕斌,伍文杰,吕晓鸣,石妍,郑磊,张建国. 125I粒子近距离治疗外放疗后复发唾液腺癌[J]. 北京大学学报(医学版), 2020, 52(5): 919-923. |
| [12] | 杨洁,张然,刘宇楠,王佃灿. 表现为耳后区巨大肿物的口外型舌下腺囊肿1例[J]. 北京大学学报(医学版), 2020, 52(1): 193-195. |
| [13] | 张旭初,张建华,王荣福,范岩,付占立,闫平,赵光宇,白艳霞. 18F-FDG PET/CT联合多种肿瘤标志物在结直肠中分化腺癌术后复发及转移中的应用价值[J]. 北京大学学报(医学版), 2019, 51(6): 1071-1077. |
| [14] | 徐帅,王旸烁,李纾,刘海鹰. 肾癌及脑膜瘤术后并发吉兰-巴雷综合征1例[J]. 北京大学学报(医学版), 2019, 51(4): 775-777. |
| [15] | 李丽伟,刘茁,王国良,张华,陈文,马静,张丽,何为,马潞林,王淑敏. 肾癌伴下腔静脉瘤栓合并血栓的多种影像学比较[J]. 北京大学学报(医学版), 2019, 51(4): 678-683. |
|
||