北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (5): 919-923. doi: 10.19723/j.issn.1671-167X.2020.05.021
125I粒子近距离治疗外放疗后复发唾液腺癌
- 北京大学口腔医学院·口腔医院,口腔颌面外科 国家口腔疾病临床医学研究中心 口腔数字化医疗技术和材料国家工程实验室 口腔数字医学北京市重点实验室,北京 100081
125I seed brachytherapy for recurrent salivary gland carcinoma after external radiotherapy
Huan-bin YU,Wen-jie WU,Xiao-ming LV,Yan SHI,Lei ZHENG,Jian-guo ZHANG( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
摘要:
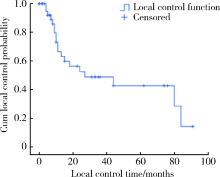
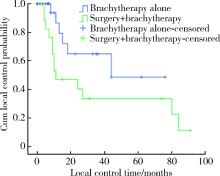
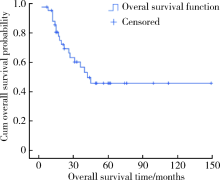
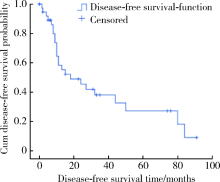
目的:探讨 125I粒子近距离治疗外放疗后复发唾液腺癌的临床应用与疗效。方法:收集2004年7月至 2016年7月收治的43例接受外放疗或手术联合外放疗后头颈部唾液腺癌复发患者,按照头颈部癌常规分割放射治疗方案(每天1次,每次1.8~2.0 Gy,每周照射5 d)计算本组患者既往累积放射治疗剂量:7例患者50 Gy以下,26例患者50~60 Gy,4例患者60~70 Gy,6例患者80 Gy以上(80~120 Gy)。患者末次外放疗至局部复发时间间隔为4~204个月,中位时间间隔为48个月。43例患者中,25例单纯行125I粒子近距离治疗,18例行手术切除后125I粒子近距离治疗,近距离治疗的处方剂量为100~140 Gy。术后随访观察,统计局部控制率、生存率及无病生存率,评价毒副反应。结果:中位随访时间27个月(2.5~149.0个月),其中,腺样囊性癌患者中位随访时间31个月(2.5~112.0个月),黏液表皮样癌患者中位随访时间18个月(5~149个月)。1、3和5年局部控制率分别为66.5%、48.8%和42.7%,生存率分别为88.0%、56.7%和45.8%,无病生存率分别为58.3%、45.4%和38.1%。单纯粒子近距离治疗组与手术切除后粒子近距离治疗组在局部控制率、生存率和无病生存率上差异无统计学意义。急性放疗反应Ⅰ/Ⅱ级2例,Ⅲ级及以上3例;晚期放疗反应Ⅰ/Ⅱ级8例,Ⅲ级及以上3例;Ⅲ级及以上放疗反应发生率为7%。结论:125I粒子近距离治疗为治疗外放疗后复发唾液腺癌提供了可供选择的治疗方法,在毒副反应发生率较低的前提下提高了局部控制率和生存率。
中图分类号:
- R739.84
| [1] |
Adelstein DJ, Koyfman SA, El-Naggar AK, et al. Biology and management of salivary gland cancers[J]. Semin Radiat Oncol, 2012,22(3):245-253.
pmid: 22687949 |
| [2] |
Zbaren P, Nuyens M, Caversaccio M, et al. Postoperative radiation therapy for T1 and T2 primary parotid carcinoma: Is it useful?[J]. Otolaryngol Head Neck Surg, 2006,135(1):140-143.
pmid: 16815199 |
| [3] |
Terhaard CH, Lubsen H, Rasch CR, et al. The role of radiotherapy in the treatment of malignant salivary gland tumors[J]. Int J Radiat Oncol Biol Phys, 2005,61(1):103-111.
pmid: 15629600 |
| [4] |
Chen AM, Garcia J, Bucci MK, et al. Recurrent salivary gland carcinomas treated by surgery with or without intraoperative radiation therapy[J]. Head Neck, 2008,30(1):2-9.
doi: 10.1002/(ISSN)1097-0347 |
| [5] | 甄鹏, 张学峰, 兰丽君, 等. 放射性125I粒子植入治疗颈部淋巴转移癌放疗后复发 [J]. 中华临床医师杂志: 电子版, 2010,4(6):810-813. |
| [6] |
Garden AS, Weber RS, Morrison WH, et al. The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation[J]. Int J Radiat Oncol Biol Phys, 1995,32(3):619-626.
pmid: 7790247 |
| [7] |
Wong SJ, Machtay M, Li Y. Locally recurrent, previously irradiated head and neck cancer: concurrent re-irradiation and chemotherapy, or chemotherapy alone?[J]. J Clin Oncol, 2006,24(17):2653-2658.
pmid: 16763279 |
| [8] | Locati LD, Perrone F, Cortelazzi B, et al. A phase Ⅱ study of sorafenib in recurrent and/or metastatic salivary gland carcinomas: Translational analyses and clinical impact[J]. Eur J Cancer, 2016(69):158-165. |
| [9] |
Hotte SJ, Winquist EW, Lamont E, et al. Imatinib mesylate in patients with adenoid cystic cancers of the salivary glands expressing c-kit: a Princess Margaret Hospital phase Ⅱ consortium study[J]. J Clin Oncol, 2005,23(3):585-590.
doi: 10.1200/JCO.2005.06.125 pmid: 15659505 |
| [10] |
Pederson AW, Haraf DJ, Blair EA, et al. Chemoreirradiation for recurrent salivary gland malignancies[J]. Radiother Oncol, 2010,95(3):308-311.
doi: 10.1016/j.radonc.2010.03.006 pmid: 20385414 |
| [11] |
Douglas JG, Koh WJ, Austin-Seymour M, et al. Treatment of salivary gland neoplasms with fast neutron radiotherapy[J]. Arch Otolaryngol Head Neck Surg, 2003,129(9):944-948.
doi: 10.1001/archotol.129.9.944 pmid: 12975266 |
| [12] |
Lee N, Millender LE, Larson DA, et al. Gamma knife radiosurgery for recurrent salivary gland malignancies involving the base of skull[J]. Head Neck, 2003,25(3):210-216.
pmid: 12599288 |
| [13] |
Salama JK, Vokes EE, Chmura SJ, et al. Long-term outcome of concurrent chemotherapy and reirradiation for recurrent and second primary head-and-neck squamous cell carcinoma[J]. Int J Radiat Oncol Biol Phys, 2006,64(2):382-391.
pmid: 16213104 |
| [14] |
Lee N, Chan K, Bekelman JE, et al. Salvage re-irradiation for recurrent head and neck cancer[J]. Int J Radiat Oncol Biol Phys, 2007,68(3):731-740.
pmid: 17379449 |
| [15] |
Haraf DJ, Weichselbaum RR, Vokes EE. Re-irradiation with concomitant chemotherapy of unresectable recurrent head and neck cancer: A potentially curable disease[J]. Ann Oncol, 1996,7(9):913-918.
pmid: 9006741 |
| [16] |
Ohizumi Y, Tamai Y, Imamiya S, et al. Prognostic factors of reirradiation for recurrent head and neck cancer[J]. Am J Clin Oncol, 2002,25(4):408-413.
pmid: 12151975 |
| [17] |
Park RI, Liberman FZ, Lee DJ, et al. Iodine-125 seed implantation as an adjunct to surgery in advanced recurrent squamous cell cancer of the head and neck[J]. Laryngoscope, 1991,101(4 Pt 1):405-410.
pmid: 1895857 |
| [18] | 江萍, 马月, 王俊杰, 等. 超声引导放射性125I粒子植入治疗头颈部复发肿瘤 [J]. 北京大学学报(医学版), 2012,44(2):291-294. |
| [19] |
Zheng L, Zhang J, Zhang J, et al. Preliminary results of 125I interstitial brachytherapy for locally recurrent parotid gland cancer in previously irradiated patients [J]. Head Neck, 2012,34(10):1445-1449.
doi: 10.1002/hed.21955 pmid: 22488812 |
| [1] | 任晓萌,李凯一,李春蕾. 基于转录组测序探索口腔扁平苔藓局部激素治疗敏感性相关分子特征[J]. 北京大学学报(医学版), 2024, 56(1): 32-38. |
| [2] | 孟令玮,李雪,高胜寒,李悦,曹瑞涛,张毅,潘韶霞. 三种方法建立大鼠种植体周炎模型的比较[J]. 北京大学学报(医学版), 2023, 55(1): 22-29. |
| [3] | 王跃,张爽,张虹,梁丽,徐玲,程元甲,段学宁,刘荫华,李挺. 激素受体阳性/人表皮生长因子受体2阴性乳腺癌临床病理特征及预后[J]. 北京大学学报(医学版), 2022, 54(5): 853-862. |
| [4] | 肖若陶,刘承,徐楚潇,何为,马潞林. 术前血小板参数与局部进展期肾细胞癌预后[J]. 北京大学学报(医学版), 2021, 53(4): 647-652. |
| [5] | 尹祯敏,王子轩,陈俊锴,孙玉春,刘云松,叶红强,周永胜. 可摘局部义齿适合性方法的评价[J]. 北京大学学报(医学版), 2021, 53(2): 406-412. |
| [6] | 张旭初,张建华,王荣福,范岩,付占立,闫平,赵光宇,白艳霞. 18F-FDG PET/CT联合多种肿瘤标志物在结直肠中分化腺癌术后复发及转移中的应用价值[J]. 北京大学学报(医学版), 2019, 51(6): 1071-1077. |
| [7] | 唐琦,林榕城,姚林,张争,郝瀚,张崔建,蔡林,李学松,何志嵩,周利群. 肾癌术后局部复发患者的临床病理特征及预后分析[J]. 北京大学学报(医学版), 2019, 51(4): 628-631. |
| [8] | 李欣欣,柳玉树,孙玉春,陈虎,叶红强,周永胜. 计算机辅助设计与制作一体化聚醚醚酮可摘局部义齿不同形态组件的适合性评价[J]. 北京大学学报(医学版), 2019, 51(2): 335-339. |
| [9] | 韩晓峰,郭曦,李铁铮,刘光锐,黄连军. 分支血管灌注不良分型在主动脉夹层腔内修复术中的应用及分析[J]. 北京大学学报(医学版), 2017, 49(6): 996-1002. |
| [10] | 王威,郑磊,刘树铭,黄明伟,石妍,吕晓鸣,张杰,张建国. 单纯放射性粒子治疗后的头颈部腺源性癌远处转移[J]. 北京大学学报(医学版), 2017, 49(3): 547-550. |
| [11] | 许挺,李民,田杨,宋金涛,倪诚,郭向阳. 超声引导下平面内经外侧肋间入路行胸椎旁阻滞的临床评价[J]. 北京大学学报(医学版), 2017, 49(1): 148-152. |
| [12] | 邢云超,熊耕砚,方东,张争,蔡林,张雷,何志嵩,李学松,周利群. 上尿路尿路上皮癌术前预后相关因素分析及初步风险分层模型构建[J]. 北京大学学报(医学版), 2016, 48(6): 1032-1037. |
| [13] | 刘余庆, 卢剑, 赵磊, 侯小飞, 马潞林. 肾移植受者上尿路尿路上皮癌术后膀胱复发的预后因素[J]. 北京大学学报(医学版), 2015, 47(4): 605-610. |
| [14] | 王威, 郑磊, 刘树铭, 黄明伟, 石妍, 吕晓鸣, 张杰, 张建国. 经手术联合125I粒子治疗唾液腺癌远处转移规律的探讨[J]. 北京大学学报(医学版), 2015, 47(3): 504-508. |
| [15] | 俞光岩, 马大权. 北京大学口腔医院唾液腺肿瘤研究50年回顾[J]. 北京大学学报(医学版), 2015, 47(1): 1-7. |
|
||